
Features
Collaboration
Leadership
Co-managing patients: RMTs can be leaders within interprofessional case collaboration
October 31, 2019 By Beth Barberree
 Photo: Getty Images
Photo: Getty Images As a health care provider (HCP), I want to do my very best to achieve the best outcomes for my patients. For me, this involves staying current with the latest research in our industry and encouraging compliance with the agreed-upon care plan. I will also refer to another RMT or HCP if patient outcomes are inconsistent with our expectations. Better yet, though, I have had great successes with patients when undertaking what I have historically called “co-managing” them in partnership with other HCPs.
As with many things in the health care realm, different words are commonly used to describe a circumstance depending on one’s clinical background and care environment. In doing background research for this article on collaborative care practices, I sourced more than one word to describe the makeup of the team and the nature of the care. For instance, “interprofessional,” “multidisciplinary,” and “interdisciplinary” are often used interchangeably. These terms essentially mean the same thing, so it would be fair to use any of them to describe a group of different professionals who work together to provide the best outcome for a patient.
Regarding the nature of care, the most common term is “co-management” in the context of institutional settings and further characterized by a formal co-management agreement. The formality of this care model is intended to delineate each HCP’s professional responsibilities and seems to focus on accountability and liability concerns.
We could instead use the term “collaborative care.” However, that term appears to have roots as the pre-cursor to a biopsychosocial approach to wellness and often refers to the involvement of a patient’s family and community. To narrow the conversation closer to the patient, I would like to settle on the term “interprofessional case collaboration” or ICC for short. This term captures the collaborative nature of shared patient care and is inclusive of both other HCPs and RMT colleagues who bring their specializations to the patient experience.
The greatest impact for patient care
Despite semantics, the heart of the matter is achieving the best possible outcomes. Research suggests ICC greatly improves the quality and safety of patient care. Constructive conversations among team members provide the advantage of their collective clinical skills and experiences; the rationale being that a higher level of service occurs with a collaborative approach than each working alone. Maybe a second assessment catches something that you did not during your initial intake. Perhaps the patient’s tissue responds better to medical acupuncture than manual techniques. So, I think we can safely say that an ICC approach does not have any risks, and is, in fact, an obvious win for the patient.
However, for all its collective knowledge, a bigger team could be perceived as a threat to the RMT who initiated the case collaboration. For instance, the patient could see another practitioner and spends less time (and money) in your clinic. Fortunately, we are each in control of our perceptions. We thus have the power to choose to see collaboration in a non-threatening manner and work on our leadership skills to shift our perspective when need be. Considering the full picture, the benefits of utilizing ICC certainly seem to outweigh the risks. Further, I would offer that failing to initiate ICC could cause financial risk for RMTs. For instance, the event that inspired me to embrace an ICC approach is as follows: A patient attended my clinic and during their first visit, they informed me they were also seeing a chiropractor. I noted to connect with the chiropractor about this patient. At their next appointment, they told me they had just seen the chiropractor, whom I had not yet spoken with, so had to rely on the patient’s description of their treatment. The chiropractor had treated the patient’s shoulder symptoms with ART. I assessed the risk of overtreating, so I chose to forego care that day. Not speaking with the chiropractor cost me clinic time (and revenue) and could have been mitigated with a simple conversation ahead of time.
To establish whether RMTs were required to collaborate, I went directly to the latest (2016) version of the Inter-Jurisdictional Practice Competencies and Performance Indicators (PCs/PIs). According to the PCs/PIs, it is identified as a competency in the first section that speaks to professionalism (1.2.r), indicating that RMTs are to “establish and maintain professional collaboration.” However, my interpretation of the four associated performance indicators does not require anything more than recognition and awareness of the value and opportunities for collaborative practice. I’ll leave the subtleties of the implications of this to the educators and regulators.
Using an ICC aproach
Based on my own clinical experience, the greatest impact of using an ICC approach is when patients have complex, often chronic presentations, and they have been working with other HCPs individually. One of the greatest assets we have as RMTs is the amount of committed one-on-one time we have with patients. I believe that this care context can lead us to discover nuggets of information and hidden secrets within the tissue that other HCPs might not. Do we not then have the professional responsibility to bring this to the attention of others?
Initiating this ICC dialogue does not have to be complicated. It can be as simple as having one other HCP on the case. If this notion intimidates you, start simple. If you have already established a network of HCPs who share a similar practice philosophy, it makes these conversations much more comfortable. If not, you can start with another RMT in your clinic or friend from school. For instance, maybe the patient whom you are treating for neck pain also has congestion in their lower extremity, so bring in an expert on lymphatic drainage.
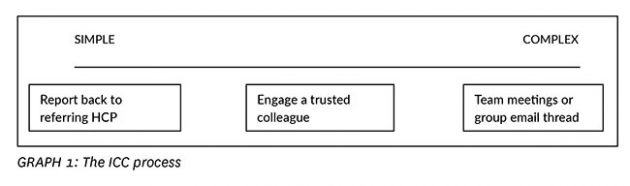
It might help to view the ICC process on a continuum (GRAPH 1). To increase the prevalence of ICC as individual RMTs, I would first encourage you to have patience. Relationship building and effective professional communication are things RMTs are generally inherently good at. Be confident in your abilities and capacity to initiate these collaborative conversations. If we start the conversation, we get to drive it and create a joint care plan with the HCPs we choose to involve and shine a light on the value we bring to the broader integrated health care team.
To easily invite the conversation about ICC with my patients, I introduced an addition to the clinic’s health history forms. It is customary to ask what other HCPs the patient is seeing, and to this, I added the opportunity for patients to consent to contact them. The option on the form opens the conversation about optimizing therapeutic outcomes and builds trust and respect in the therapeutic relationship, and can be reinforced during the discussion while obtaining consent to treat, considering the treatment plan, and at what point I would refer to another HCP. Of course, each jurisdiction will have its practice guidelines, so please be mindful before implementing any strategies into your practice.
Not everyone you reach out to will reply. When I encounter this, I choose to believe that it is not a professional slight, but rather a symptom of time pressures we all too often experience. Indeed, some HCPs hold RMTs in less high regard than other HCPs. I see this improving year by year, which is encouraging and I believe due in large part to the tremendous advocacy undertaken by our professional associations across the country. Other health professions are embracing collaborative practice at a foundational level. For instance, the College of Physicians of Alberta recently updated its strategic priorities to “increase collaboration with other healthcare professionals to improve patient care…”
Part of our ongoing growth as health professionals is being able to be reflective and consider honestly where our areas for growth are. I would challenge you to think whether you believe ICC would be of value to your patients and you, as a health care professional. If so, seek out opportunities to build your skills in this realm and be a leader of interprofessional case collaboration in your practice.
Beth Barberree, rmt has been a massage therapist since 1995. She has spent many years championing high practice standards and advocating for regulation of massage therapy in Alberta, initially as President of the Massage Therapist Association of Alberta (2002-2007) and most recently as the founding Chair of the Alberta Support Council for Massage Therapy.
Print this page