
Health News
Iliopectineal Bursitis
Do you or your patients or clients suffer from anterior hip joint pain, especially with any physical exertion? This could be as a result of irritation to the iliopectineal bursae, which is usually due to tight hip flexors (Iliopsoas, Rectus Femoris) and a tight hip joint capsule.
October 1, 2009 By Mike Dixon RMT
General Discussion
Do you or your patients or clients suffer from anterior hip joint pain, especially with any physical exertion? This could be as a result of irritation to the iliopectineal bursae, which is usually due to tight hip flexors (Iliopsoas, Rectus Femoris) and a tight hip joint capsule.
Although there are many conditions that cause anterior hip and thigh pain like hip degenerative arthritis, femoral nerve entrapment, lumbar facet syndrome and inguinal hernias; a simple cause is iliopectineal bursitis.
 This article will focus on the etiology, anatomy, kinesiology, clinical signs and symptoms, assessment and a few treatment techniques for manual therapist.
This article will focus on the etiology, anatomy, kinesiology, clinical signs and symptoms, assessment and a few treatment techniques for manual therapist.
Etiology:
Friction trauma from muscle hypertonicity – common in cross country skiers, kickers, dancers, gymnasts and long distance runners.1
Anatomy/Kinesiology
The hip joint capsule is composed of three very strong ligaments (iliofemoral, pubofemoral and ischiofemoral). The strongest is the iliofemoral, sometimes described as the Y ligament of Bigelow as it looks like a inverted Y.
These ligaments are such that they twist and compress the joint with every step or stance phase of gait. This action compresses the articular cartilage and thus bathes the articular surfaces in synovial fluid. The synovial membrane of the hip joint lines the fibrous layer of the capsule. The synovial “cavity” often communicate anteriorly with the iliopectineal bursa.2
This is interesting to note as synovial fluid can travel from the joint capsule to the bursae and vice versa. This means that with joint irritation, degenerative joint disease or synovial effusion, the bursae may also become swollen or irritated.
There are three clinically significant bursae surrounding the hip (out of 18); they are the Trochanteric, Ischiogluteal and Iliopectineal or iliopsoas bursae.
The rather large iliopectineal bursa overlies the anterior aspect of the hip joint and the pubis and lies beneath the Iliopsoas muscle as it crosses in front of the hip joint.
This bursa often communicates with the hip joint anteriorly through a space between the Pubofemoral
and Iliofemoral ligaments. This may be a factor in the characteristic anterior pain experienced by patients with hip joint disease.3
Assessment:
A. Key history taking/red flags:
1. How would you describe your level of activity?
Athlete versus weekend athlete. Are there any periods of prolonged sitting or inactivity? Periods of prolonged sitting followed by physical exertion can shorten the Psoas muscle and may contribute to the bursae irritation.
2. Any previous hip injuries or leg length differences?
This could lead to secondary arthritis, which can contribute to the bursa swelling.
3. Can you identify the site of irritation?
The patient can usually identify the site of the pain in or about the inguinal ligament but pain can radiate to the low back, thigh, gluteal area or even the knee.
4. Is there an increase in pain with weight bearing activity like walking, running, hiking, kicking or hip stretching?
There is usually an increase in pain with these activities.
5. Does the hip pain increase or radiate into the leg(s) with coughing, sneezing or strained bowel movements?
If the answer is yes to any of the above questions, this is a red flag. The problem may be related to other pathologies like inguinal hernias, disc injuries or space occupying lesions. The patient should then be referred to a physician.
B. Observation:
Observe patient’s gait and standing posture for obvious abnormalities.
(guarded or antalgic gait, increased pelvic angle and heights, sway back, lumbar scoliosis)
C. Palpation:
There may be localized tenderness anteriorly if the iliopectineal bursa is inflamed or distended. The iliopsoas muscles may be tender and sensitive or painful to the touch.4
D. Range of motion assessment:
A full range of motion assessment should be done both in closed kinetic and open kinetic chains (weight
bearing and non weight bearing). Perform your active range of motion, followed by passive with passive overpressures to determine the joint endfeels. All endfeels should be capsular except hip flexion which is soft. Resisted motion assessment and appropriated selective muscle testing to determine muscle imbalances. If a capsular pattern of restriction is present, there may be joint effusion and or osteoarthritis/capsular fibrosis.
Key finding: There will likely be pain and weakness with resisted hip flexion and localized pain with passive hip extension, as both motion tests will compress the bursa.
For Your Reference:
“Active Range of Motion:
Flexion: 120 degrees
Extension: 30 degrees
Abduction: 45 degrees
Adduction: 30 degrees
Lateral rotation: 45 degrees
Medial rotation: 35 degrees
Capsular Pattern of Restriction
Flexion, Abduction, and Medial Rotation > Extension, Adduction and Lateral Rotation.5
E. Neurological and referred pain:
The low back should be examined for nerve root involvementExamine the L1, L2, L3 dermatomes for sensory loss and reflexes of L4 and S1 (Patella, Achilles) The femoral nerve (L2-4) may also be compressed under the inguinal ligament when the bursa swells narrowing the space between the hip joint and the inguinal ligament.
 Special tests: There are a few key special tests that can be performed to confirm iliopecteal bursitis or differentiate other conditions. In truth, by the time you have performed your active, passive and resisted testing you should be well on your way to confirming this condition. The four special tests I have chosen to confirm this condition are as follows:
Special tests: There are a few key special tests that can be performed to confirm iliopecteal bursitis or differentiate other conditions. In truth, by the time you have performed your active, passive and resisted testing you should be well on your way to confirming this condition. The four special tests I have chosen to confirm this condition are as follows:
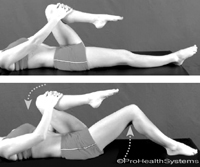
Thomas test: To show shortening hip flexors. This test is usually positive.
Procedure: Supine patient flexes on knee to chest while keeping the other leg straight, the examiner observes
for straight leg elevation.6
Patrick Faber’s test: To show shortening of the adductors, flexors and hip joint capsule and any sacroiliac involvement. Test is usually positive.
Procedure: Patient supine, examiner instructs patient to cross legs into a figure 4 position (ankle placed above contralateral knee), examiner then stabilizes pelvis and applies gentle downward pressure over the flexed knee.7
 Femoral Nerve Stretch test (Yeoman’s):
Femoral Nerve Stretch test (Yeoman’s):
To show any involvement of the femoral nerve. This test should be negative unless the bursae is pressing on the nerve.
Procedure:
Patient prone with knee flexed 90 degrees, with one hand examiner applies downward pressure over the PSIS, lifts patient’s knee off examining table and try to extend the thigh with the other hand.8
 Scour Test:
Scour Test:
For joint degeneration, which may be a co-existing condition. This test should be negative, however, the patient will complain of a pinching feeling in the hip joint crease with the test position of flexion, adduction and internal rotation. You may have already discovered this during you range of motion assessment.
Procedure:
The examiner flexes and adducts the patient’s hip so the hip faces the patient’s opposite shoulder and resistance to the movement is felt. As slight resistance is maintained, the hip is taken into abduction while maintaining flexion in an arc of movement.”9 (Perform with care!)
Treatment/Management:
In the sub-acute and chronic state of the condition, what I have found to be very helpful is:
- Manual stretch and trigger point release of the Iliopsoas, Iliacus and Rectus Femoris.
- Active Release techniques for
the hip flexors. Lateral and axial distractions, grades 2-3 sustained glides and grades 3-4 oscillations.
 Treatment frequency:
Treatment frequency:
usually 1-2 per week for 6-8 weeks. Providing hip flexor stretching exercises and strengthening the abductors to create hip/pelvis stability.
Other suggestions:
• Ice or cold applications to the affected area after activity or when irritation or swelling is present.
• Ultrasound/interferential may be used to reduce inflammation and swelling.
References:
- Quick reference clinical Chiropractic Conditions Manual, Page 148. By Nikita Vizniak DC
- Page 288, Management of Common Musculoskeletal Disorders, 3rd edition
- Page 289, Management of Common Musculoskeletal Disorders, 3rd edition
- Page 296, Management of Common Musculoskeletal Disorders, 3rd edition
- Reference: Joint Play the Right Way 2nd edition, page 126
- Quick reference clinical Chiropractic Conditions Manual. By Nikita Vizniak, 2nd edition, page 239
- Quick reference clinical Chiropractic Conditions Manual. By Nikita Vizniak, 2nd edition, page 237
- Quick reference clinical Chiropractic Conditions Manual. By Nikita Vizniak, 2nd edition, page 185
- Orthropedic and Physical Assessment 4th edition, pages 642, 643
References:
• Joint Play the Right Way for the Peripheral Skeleton, by Mike Dixon RMT
• Quick reference clinical Chiropractic Conditions Manual 1st & 2nd editions. By Nikita Vizniak, DC
• Management of Common Musculoskeletal Disorders, 3rd edition, by Hertling & Kessler
• Orthropedic and Physical Assessment 4th edition, by David J. Magee
Mike Dixon, RMT is the Author of Joint Play the Right Way for the Peripheral Skeleton 1st and 2nd editions. Mike has been teaching clinical orthopaedics at the West Coast College of Massage Therapy for the past 13 years and offers continuing education in Arthrokinetic Therapy. website: www.arthrokinetic.com
Print this page