
Features
Patient Care
Practice
Essentials of Assessment: Summer 2005
After specific impairments related to an injury or condition have been or are on their way to being resolved, the therapist needs to shift from a local focus and move to a more global view.
September 29, 2009 By David A. Zulak MA RMT
After specific impairments related to an injury or condition have been or are on their way to being resolved, the therapist needs to shift from a local focus and move to a more global view.
The therapist needs to ensure that the compensatory structures and tissues have not only been addressed in the acute and chronic stages, but as the principle impairments resolve, that all tissues are being re-integrated into the whole body.
 This requires that all structures and tissues are physiologically and functionally working as optimally as possible. In other words, the therapist seeks to remove all impediments, as far as is possible within our scope of practice.
This requires that all structures and tissues are physiologically and functionally working as optimally as possible. In other words, the therapist seeks to remove all impediments, as far as is possible within our scope of practice.
This is where the “body scan” can be placed, in the assessment protocol, and where it can be most useful. The first goal is to find out what needs to be done in order to re-integrate a previously injured body. The second stage is to find predisposing factors that may lead to re-injury or future dysfunctions.
Let’s use the example of a patient recovering from a second degree ankle sprain that originally involved the anterior talofibular ligament (ATFL) and the calcaneofibular ligament (CFL). Also involved were the peroneals/fibularis muscles.
These will have been injured while eccentrically contracting to protect the ankle. The lateral portion of
the subtalar joint sustained some degree of injury as well.
Several weeks following the injury, the patient is ready to accelerate their activities. The tissues have been healing well because the patient has been compliant with attending treatments and home care.
While there is improving strength in the musculature, the function of the foot and lower leg requires re-training. Some of the re-training will include active free range of motion, both weight and non-weight bearing, and possibly a wobble board to improve the proprioception in and around the ankle.
The patient also needs to reduce compensatory holding and guarding patterns. Some of this needs to be addressed by the therapist, and some through home care. It is at this point that a whole body, or at least a lower body scan, can be of great use.
As the name implies, a scan is meant to be global in nature. To see how some parts of the whole are functioning individually in a general way, and how they are all working together collectively. The therapist needs to do just enough testing of each joint to tell how well it may be contributing to, or preventing, appropriate function of the each limb (lower or upper), along with its associated girdle, (pelvis or shoulder), and that portion of the spine most affected by those limbs & girdle.
The therapist should begin by doing a brief postural assessment by checking the basic landmarks of the body, noting any asymmetries. If you have the room, have the patient walk back and forth 10 steps or so to observe gait or motion abnormalities.
 A standing flexion test can be done to look for scoliosis, sacroiliac joint dysfunctions, and general flexibility and stability of the low back. Also side-bending and rotation of the torso is informative about spinal column and ribs. This is informative in that it will let you know if further specific testing should be pursued.
A standing flexion test can be done to look for scoliosis, sacroiliac joint dysfunctions, and general flexibility and stability of the low back. Also side-bending and rotation of the torso is informative about spinal column and ribs. This is informative in that it will let you know if further specific testing should be pursued.
This is also a good time to have the patient abduct their arms up over their heads and have them try to touch the back of their hands together overhead. This action will not only let you observe the general mobility of the shoulder girdle, but demands that the forearms supinate.
Observe the clavicles before, during and after movement to help check symmetry of movement, and/or for sternoclavicular or acromioclavicular dysfunctions. Observe whether the thumbs are beside each other and as high as the other when the arms are overhead. Note how flexed the elbows need to be in order for the back of the hands to touch, and as with all observations, the asymmetries between bilateral structures.
These tests will take less than three minutes to perform.
To check for range of motion restrictions and muscle imbalances, have the patient lie supine. A quick neurological check for lumbar nerve roots, combined with muscle testing of the lower joints in general, takes no more than a couple of minutes. Have the patient lay with their knees bent (“crook lying” – this also safeguards the low back). Stand at the end of the table, by their feet.
Tell them to lift the front of both feet off the table, while leaving the heels on the table. You can do the following bilaterally: tell the patient not to let you move their ankles/feet as you press down on the dorsum of the feet (testing L4), and then slip further along and press down on the toes. (Testing L5 specifically – you can also passively extend their big toe and then have the patient resist as you press down on the big toes, to be thorough). Then try everting, inverting (you will be testing S1) and dorsiflexing the feet against the patient’s resistance to your attempts to move them.
Ask the patient to now lift the heel off the table while you grasp the calcaneous and have them resist as you try to extend the leg, (testing S1-2). You may find it best to do this one leg at a time, as the strong hamstrings require a good pull to be adequately tested.
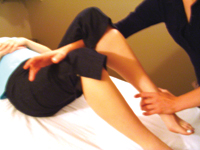
Move to the side of the table at their knee. Lift their leg until you can slip your forearm under their knee and place the distal forearm just above their patella.
The foot on that side will remain off the table. Lift their leg until the knee is bent 50 to 60 degrees. Grasp the leg just above the ankle. Tell the patient to resist you trying to bend the knee and then try to push the heel of the foot towards the table, (L3-4). Position your self so that you can safely push down without hurting yourself.
Move to the patient’s chest and ask them to lift their foot approximately 12 inches off the table as you place your two hands just above the knee. Try to push the foot to the table to test the hip flexors. To test specifically for the psoas, flex the hip to 90 degrees and again try to push the foot to the table, (L2).
 Next, move around the table and test the other knee extensors and hip flexors. Practice once or twice and you will find this a fast and accurate testing of muscle groups and lumbar nerve roots. Another minute or two taken, at most.
Next, move around the table and test the other knee extensors and hip flexors. Practice once or twice and you will find this a fast and accurate testing of muscle groups and lumbar nerve roots. Another minute or two taken, at most.
Note: By extending the big toes as above, you will have been able to observe whether they have the minimal 35-45 degrees of extension, (normal is 75-90), which is the minimal requirement for proper toe-off during walking.
Now joint mobility can be tested passively. Have the patient relax, as they lay supine. If the patient is not experiencing any low back pain, have the legs extended to begin.
Lift one leg and with one hand dorsiflex, plantar flex, evert, and invert the foot. Complete the ankle testing with circumduction.
Grasp the distal metatarsals and supinate and pronate the forefoot. Flex and extend the toes.
Try to perform these tests without stopping, creating a smooth flow with each reposition of your hands.
Test the knee: shift your hold with one hand above the knee and the other at the calcaneous; then fully flex the knee.
With the hand that is under the foot grasping the calcaneous, rotate the tibia externally and internally.
This motion will specifically test the posterior surfaces of the meniscus while it tests for full flexion of the knee. You can then move right into McMurry’s meniscus test for lateral and medial meniscus. Extend the knee to 5 degrees of flexion and test the lateral and medial ligaments of the knee, and test again at full extension. Lift the extended leg to check the length of the hamstrings.
Moving on, Flex the hip fully, then bring back to roughly 90 degrees and using the lower leg (if no knee pathology is found) and internally and externally rotate the hip. (Pain and or loss of internal rotation of the hip can be the first sign of a capsular pattern of restriction.) Now, place the leg in Faber’s (Patrick’s or Figure 4 test) to test abduction (and the length of the adductors), along with the Sacroiliac joint. Lift the knee up towards the ceiling and then slightly across the table to test adduction (and the length of the abductors).
You can place the foot of the leg you are testing on the far side of the other leg which is on the table, to accentuate the test of passive adduction of the hip. Finish with circumducting the hip.
Have the patient turn onto their side and then take the upper leg into extension to test the range of extension at the hip. Have them lay supine again, and move to the other side of the table to test the opposite knee and hip.
At this point you have performed quick and efficient scan of the lower body. You will know if any areas of the lower body require treatment to be reintegrated into a working whole. You may also find areas that require treatment due to the cumulative trauma caused by compensation.
The scan can be continued to include the upper extremity. This can be done side-lying leaving the elbow flexed: take the shoulder into flexion, then resist as you have the patient try to extend the shoulder; next, take the shoulder into extension, then resist as you have the patient try to flex the shoulder.
Now, take the shoulder into abduction (no humeral rotation, pure glenohumeral) … resist adduction … adduction … resist abduction … internally rotate … resisting … external … Finish by placing the hand behind the low back.
 In side-lying, you can easily have the patient fully relax as you circumduct the humerus once/twice in the glenoid fossa. If there is no pain, add a compressive force to accentuate the testing of the joint surfaces. Now, traction the arm straight up and circumduct to test the joint capsule during stretch.
In side-lying, you can easily have the patient fully relax as you circumduct the humerus once/twice in the glenoid fossa. If there is no pain, add a compressive force to accentuate the testing of the joint surfaces. Now, traction the arm straight up and circumduct to test the joint capsule during stretch.
The shoulders should take no more than a minute or so each to test.
If you stabilize the scapulae by holding it over the acromion, you can make the above shoulder movements specific to the glenohumeral joint. These are known as “Spenser’s mobilizations.” The latter is used in Osteopathic Manual Therapy.
This series of mobilizations is used to assess, AND re-balance the muscles that govern the specifics movements of the glenohumeral joint.
In adding isometric resistance during range of motion testing, you can lengthen tight/taut antagonists that are restricting motions, and begin restoring muscle balance around the joints. Hence, assessment and treatment can begin to merge here.
To return to the full body, or upper body scan, you can quickly check the range of motions of the elbow and wrist in a similar fashion, either still in the side-lying position or wait till you have done the other shoulder and then do them in a supine position.
Next, the motions of the cervical spine can be assessed.
In summary, this, or a similar pattern of testing, can be done quickly and provide a great deal of information about how the patient is presenting at that time. You will be able to evaluate how treatments have gone so far, and plan where they may need to go next.
Assessment done during the body scan has the purpose of determining where and how to reintegrate previously injured or dysfunctional segments of the body back into the whole. Testing itself can be helpful by actually treating, in the early stages of, that very re-integration process.
With the simple addition of isometric testing and repetition of isometric resistance, not only done in mid-range, but especially at restricted end-ranges (post isometric relaxation), the above scanning actions will be assisting in re-tuning of muscle balance and function.
Doing a scan of the whole body, or of the lower/upper, can quickly and easily be turned into a technique for re-integrating the parts of the body back into a complete, co-ordinated whole. The patient almost always finds scanning in this manner to be; very comfortable, often relaxing and restorative, as well as informative.
Print this page