
Features
Practice
Technique
Carpal Tunnel
A few years ago a client of mine was diagnosed as having carpal tunnel syndrome (CTS) by a neurologist. Surgery was recommended in six months if the symptoms stayed the same, but she wanted to try other therapeutic interventions before going this route.
September 28, 2009 By Fiona Rattray Rmt
A few years ago a client of mine was diagnosed as having carpal tunnel syndrome (CTS) by a neurologist. Surgery was recommended in six months if the symptoms stayed the same, but she wanted to try other therapeutic interventions before going this route.
 Classic carpal tunnel symptoms initially include numbness and tingling in the lateral three and a half digits (thumb, index, middle and half the ring finger) – often worse – with movement or at night. Activity, such as repetitive flexion and extension, increases wrist pain. CTS may present unilaterally or bilaterally; if only one hand is affected, it’s usually the dominant one. Over time, CTS symptoms of numbness, pain, limited wrist movement, muscle weakness and swelling can progress to atrophy of the thenar muscles.
Classic carpal tunnel symptoms initially include numbness and tingling in the lateral three and a half digits (thumb, index, middle and half the ring finger) – often worse – with movement or at night. Activity, such as repetitive flexion and extension, increases wrist pain. CTS may present unilaterally or bilaterally; if only one hand is affected, it’s usually the dominant one. Over time, CTS symptoms of numbness, pain, limited wrist movement, muscle weakness and swelling can progress to atrophy of the thenar muscles.
Repetitive wrist actions can lead to edema and chronic fibrosis. As the tendons thicken, the available space in the tunnel is reduced.
Some people are susceptible to CTS due to the presence of systemic conditions leading to connective tissue degeneration or edema, such as with diabetes mellitus or during pregnancy.
Previous fractures or dislocations at the wrist may reduce the space available in the tunnel. A wrist that is more square than rectangular in cross-section, which also reduces tunnel space, may lead to CTS when combined with an occupation that stresses the wrist.
Pressure inside a healthy carpal tunnel with the wrist in a neutral position is 2.5 mmHg, rising to 31 mmHg on full flexion or extension. In the case of CTS,
this resting pressure is 32 mmHg, rising to well over 90 mmHg on full flexion or extension. Put a blood pressure cuff around your arm and inflate it to this pressure and it’s easy to understand the compressive forces on the tunnel contents when CTS is present.
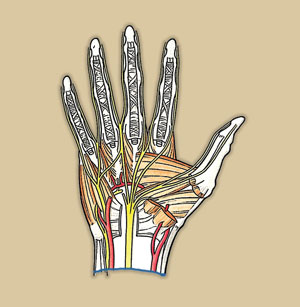
Reviewing the pertinent anatomy, the carpal tunnel lies just distal to the wrist creases. The carpal bones form the floor of tunnel, while the roof is the transverse carpal ligament. This dense, tough fibrous band, approximately 2 mm thick, attaches to the scaphoid tubercle and the trapezium on the radial side, and the hook of the hamate and the pisiform on the ulnar side.
Through the tunnel pass the median nerve, the four tendons of both flexor digitorum superficialis and profundus, and the tendon of flexor pollicis longus.
Just before it goes through the carpal tunnel, the median nerve gives off a branch called the palmar cutaneous nerve, which travels over, not through, the carpal tunnel. This is significant because the palmar cutaneous nerve, supplying the skin over the thenar eminence, won’t be affected by CTS.
Classic Phalen’s Test For CTS
Ask the client to put the backs of the hands together, with wrists flexed, elbows held horizontally and the shoulders not elevated. Then instruct the client to strongly compress the backs of the hands together for one minute which produces maximum compression on the structures within the carpal tunnel. Reproduction of the client’s symptoms in thumb, index finger, middle finger and lateral half of the ring finger are positive for CTS.
A variation of this is the Reverse Phalen’s Test, where the client puts their palms together, strongly compressing them for one minute. Tingling or pain reported as in the test above is also positive for carpal tunnel syndrome.
 Thinking Outside The CTS Definition
Thinking Outside The CTS Definition
At odds with the classic CTS symptoms, my client also had numbness and pain in her hypothenar eminence, little finger and the flexor surface of her arm from elbow to wrist. She had neck pain, too; a head-forward posture and protracted shoulders were obvious.
Perhaps because CTS is well-known and accepted as a condition by the medical model and the public, the focus often stops on the carpal tunnel when hand symptoms are mentioned. For example, symptoms that affect the ring and little finger may be mistakenly reported by the client as CTS.
But there are a number of other structures proximal to the carpal tunnel that could also be compressing the nerves and vasculature supplying the arm and hand. These structures should be investigated as possible contributors to the client’s condition.
They include cervical vertebrae, ribs, clavicle, and muscles such as scalenes, pectoralis minor, subclavius and pronator teres. Tight fascia of the anterior neck, chest and arm can exert compressive forces.
Trigger points in muscles such as the scalenes or subclavius can refer pain and other sensations into the hand. Acute tendinitis at the elbow (extensor or flexor tendons) or thumb (abductor pollicis longus and extensor pollicis brevis) may refer forearm and hand pain. Thoracic outlet syndrome has three possible locations for brachial plexus compression: between anterior and middle scalenes (anterior scalene syndrome), between coracoid process and pectoralis minor (pectoralis minor syndrome) or between the clavicle and first rib (costoclavicular syndrome).
- When CTS occurs in combination with compression proximal to the wrist it’s called double crush syndrome.
- Pronator teres syndrome is compression of the median nerve near the proximal attachment of pronator teres. The client experiences gradual aching and heaviness in the anterior forearm, and numbness in the thumb and index finger. Pain occurs with repetitive elbow movement, but there are no nocturnal symptoms (Schumacher, 1993).
- A cervical rib at C7 may be present for some people. This cervical rib may be a partial cartilaginous projection from the C7 transverse process, or may form a complete cervical rib connecting to the first thoracic rib. This narrows the depth of the interscalene triangle between middle and anterior scalene, compressing the neurovascular bundle.
The rib may have shown up on an x-ray, or may be palpated as a bulge between the scalenes at the level of the clavicle. Thoracic outlet syndrome is present for about half of those with a cervical rib.
Vertebral Artery (VBA) Test
Rule out vertebral artery circulation deficiency at the transverse foramen before doing other neck tests. Ask the seated client to rotate the head fully to one side, and then extend the neck, holding this position for 30 seconds. Repeat on the other side. If the client experiences dizziness or nystagmus (an involuntary, repetitive, circular motion of the eyes) or both, the test is positive and the client should be referred to a physician for VBA assessment (Gerard, Kleinfield, 1993).
Valsalva’s Test
This test has fallen into disfavour as it may cause post-test dizziness or syncope in those clients with cardiac pathologies. Pressure within the spinal column – due to a herniated disc or osteophytes – is further increased by asking the client to bear down, as if moving the bowels. This action increases venous backpressure, with pain local to the lesion site or radiating in a dermatomal pattern. Instead of performing the test, just ask the client if pain occurs when coughing or sneezing.
Spurling’s Test
Assess for cervical nerve root compression or facet joint irritation with this test. Stand behind the seated client. Ask them to slowly extend, sidebend and rotate the head to the affected side. Carefully apply compression downward on the client’s head. The combination of head position and downward pressure compresses the intervertebral foramen, the nerve root and the facet joints on that side. Radiating pain or other neurological signs down the affected arm are positive signs for nerve root involvement. Pain remaining local to the neck or shoulder indicates cervical facet joint irritation on the side being tested (Gerard, Kleinfield, 1993). Avoid this test if the vertebral artery test is positive.
Slump Test
Check for nerve root involvement, dural or meningeal irritation with this test. Have the seated client put both hands behind the head; pull the chin to chest, allowing the thoracic and lumbar spine to slump into flexion. Next, ask the client to extend one knee and dorsiflex that ankle, holding the position. The same actions are repeated with the other leg, fully stretching the dural tube and spinal cord. A positive test is pain along the spine and perhaps referred into a limb. This occurs at the spinal level of the lesion (Hertling, Kessler, 1996).
Upper Limb Tension Tests
These 4 tests determine whether cervical nerve roots and peripheral nerves are the source of shoulder or arm pain. Peripheral nerves and nerve roots are stretched, similar to the straight leg raise test. Specific nerves are stressed depending on arm, elbow and wrist position. These tests are useful when restricted shoulder ROM makes tests requiring full ROM – such as Adson’s and Wright’s – difficult to perform.
The starting position is the same: the client is supine, close to the side of the table, with head turned away from the side you’re testing. Apply a constant pressure with one hand, depressing the client’s shoulder. Your other hand holds the client’s wrist and moves the arm into positions described below. In all cases, pain or symptom reproduction is a positive test (Magee, 1997).
Upper Limb Tension Test 1 (C5, C6, C7 and median nerve)
Abduct the humerus to 110 degrees,extend the humerus to 10 degrees below the coronal plane and externally rotate the humerus to 60 degrees. (At this point, a stretching sensation is normally experienced across the anterior shoulder.)
Next, slowly extend the wrist, then the fingers. (Tingling is normally experienced in the lateral three digits.) Last, fully supinate the forearm, then slowly extend the elbow. (A stretching sensation is normally experienced in the anterior elbow.)
Upper Limb Tension Test 2 (median, musculocutaneous and axillary nerves)
Abduct the humerus to 10 degrees. Slowly extend the wrist, then the fingers. Last, fully supinate the forearm and slowly extend the elbow. (Tissue tightness in the shoulder or elbow, or tingling in the fingers is a normal response.)
Upper Limb Tension Test 3 (radial nerve)
Abduct the humerus to 10 degrees. Slowly flex the wrist and fingers and deviate them ulnarly. Last, fully pronate the forearm and extend the elbow.
(As before, tissue tightness and tingling are normal.)
Upper Limb Tension Test 4 (C8 and T1 nerve roots and radial nerve)
Abduct the humerus to 90 degrees. Flex the elbow, bringing the hand towards the client’s ear. Supinate the forearm. Last, slowly extend the wrist and
fingers and deviate them radially. (As before, tissue tightness and tingling are normal.)
First Rib Mobility Test
Check the mobility of the first rib by starting with the client in a seated position. Have the client rotate the head fully away from the affected side and then flex the head forward to the chest as far as possible. A positive test for first rib hypomobility is indicated by limited flexion. Scalene hypertonicity or fascial restrictions may cause the hypomobilty. A cervical rib, if present and contributing to decreased mobility, may be palpated as a bulge between middle and anterior scalenes at the level of the clavicle.
Active trigger points in the anterior scalene muscle are revealed by the following test. Ask the seated client to put the forearm on the affected side across the forehead, as close to the elbow as possible. Then, have the client elevate and protract the shoulder, lifting and clavicle and relieving any compression of the scalenes and brachial plexus. Reduction of pain within a few minutes is a positive test for active trigger points. However, pain due to a cervical radiculopathy is not reduced (Travell, Simons, 1983).
Adson’s Test
Assess for thoracic outlet syndrome caused by the anterior scalene muscle with this test. Stand behind the seated client. Extend and slightly externally rotate the client’s affected arm while monitoring the radial pulse. Next, ask the client to rotate the head towards the affected side, and take a deep breath, holding it for at least 15 to 20 seconds. The first rib is elevated, compressing the neurovascular bundle against the tight anterior scalene muscle. A positive test is indicated by a diminished radial pulse or recurrence of the client’s symptoms (Travell, Simons, 1983).
Travell’s Variation On Adson’s Test
To determine if middle scalene is
the cause of thoracic outlet syndrome, start by standing behind the seated client. Extend and slightly externally rotate the client’s affected arm as in Adson’s test, while monitoring the radial pulse. Instruct the client to rotate the head away from the affected side and to take a deep breath, holding it for at least 15 to 20 seconds. The first rib is elevated, compressing the neurovascular bundle against the tight middle scalene muscle. Diminishment of the pulse or recurrence of the symptoms indicates a positive test for medius scalene involvement (Travell, Simons, 1983).
Wright’s Hyperabduction Test
To assess pectoralis minor as the possible cause of thoracic outlet syndrome, stand behind the seated client. Monitor the client’s radial pulse, fully abduct the arm to 180 degrees and then slightly extend the arm. This places a stretch on the brachial plexus and axillary artery as they pass inferior to the pectoralis minor muscle. A diminishment of the radial pulse or recurrence of the client’s symptoms is positive for a tight pectoralis minor muscle
Costoclavicular Syndrome Test
Check for thoracic outlet syndrome due to compression by the clavicle with the following test. Stand behind the seated client and monitor the radial pulse. With your other hand, depress and protract the affected shoulder. A positive test is indicated by a diminished pulse or an increase in symptoms.
 4 Muscle Length Tests
4 Muscle Length Tests
Shortened shoulder protractors and humeral adductors may also cause compression of the neurovascular bundle. The following four tests can be done in sequence with the client lying supine. You stand at the head of the table.
Pectoralis Minor Length
Using both acromioclavicular joints as landmarks, observe for shoulder protraction on the affected side, since pectoralis minor protracts the scapula. A protracted shoulder is higher off the surface of the table.
Pectoralis Major Length
Pectoralis major has two main divisions: the clavicular (or superior) fibres, and the sternal (or inferior) fibres. Have the client slide to one side so that the shoulder is at the edge of the table. Ask that the arm be placed at 90 degrees of abduction to check the clavicular fibres, and then be placed at 150 degrees of abduction to check the sternal fibres. Have the client slide to the other side of the table and repeat. In both abduction positions, pectoralis major is short if the arm does not drop below the level of the table into extension and external rotation.
Latissimus Dorsi/Teres Major Length
With the client back in the centre of the table, ask the client to first flex the hips and knees, putting the plantar surface of both feet flat on the table; then, to flatten the low back against the table so the pelvis is in posterior pelvic tilt, fixing the lumbar attachment of latissimus dorsi. Now have the client raise both arms above the head, through full flexion at the glenohumeral joints. If latissimus dorsi/teres major are short, the posterior surface of the affected arm(s) will not contact the table above the client’s head (Kendall et al., 1993).
Extensor Tendinitis Test
The client is seated, with the elbow in extension and the wrist in pronation and slight extension. Ask the client to hold the wrist in this position, and then you attempt to flex the wrist. Pain at the common extensor tendon and weakness are positive signs for tendinitis. To isolate extensor carpi radialis brevis, which is often the source of extensor tendinitis pain, have the client’s elbow in flexion, wrist in pronation and slight extension. Proceed as above with the client resisting wrist flexion. Pain and weakness are positive signs.
Flexor Tendinitis Test
The client is seated, with the elbow in extension and the wrist in supination and slight flexion. Instruct the client to hold the wrist in this position, and then you attempt to extend the wrist. Pain at the common flexor tendon and weakness are positive signs for tendinosis.
Pronator Teres Test
To check for pronator teres syndrome, the client is supine. You stabilize the client’s elbow against their torso with one hand. Holding the client’s arm just proximal to the wrist with the other hand, partially flex the client’s elbow, and pronate the forearm. Ask the client to hold the wrist in this position, and then you attempt to supinate the forearm (Kendall et al., 1993). Pain inferior to the medial epicondyle and numbness in the thumb and index finger are positive signs.
Finger Flexion Test
Another test for active trigger points in the scalene muscle group starts with asking the client to hold the metacarpophalangeal joints of the affected side in full extension. Next, ask the client to flex the interphalangeal joints, attempting to touch the fingertips to the palmar surface over the metacarpophalangeal joints. (The client should not make a fist.) If all four fingertips cannot touch the metacarpophalangeal joints, a positive test for active scalene trigger points is recorded (Travell, Simons, 1983).
Finkelstein’s Test
To determine the presence of deQuervain’s tenosynovitis, ask the client to make a fist of the affected hand, with the thumb firmly held in flexion inside the flexed fingers. Instruct the client to ulnarly deviate the wrist, keeping the thumb and fingers flexed in a fist. Sharp pain along the abductor pollicis longus and extensor pollicis brevis tendons at the wrist is positive for tenosynovitis.
AR Test of Abductor Pollicis Brevis
To assess for the strength of abductor pollicis brevis, which may be weak with median nerve compression, do the following test. Supinate the client’s forearm and fully abduct the thumb. Ask the client to hold this position. Place pressure on the proximal phalanx of the client’s thumb and attempt to adduct it. Weakness is a positive test.
Proceeding To Treatment
Record the positive tests. You may indeed find that your client has CTS in isolation. If so, the treatment plan for decreasing median nerve compression at the carpal tunnel should be followed. However, it’s quite possible that you’ll discover a double crush syndrome, or perhaps no CTS at all, but scalene trigger points or thoracic outlet syndrome.
In the case of my client, she had short, tight middle scalenes and pectoralis minor, a classic thoracic outlet syndrome in addition to a mildly positive Phalen’s test. The fascia over her anterior neck and pectoral region was very tight. Additional complications were hypermobile carpal bones, and extensor tendinitis. Dynamometer readings showed her grip strength to be markedly weaker in her dominant hand. We worked out a treatment plan which gave time
for me to address these areas over a three-month period.
She was diligent and motivated in doing self-care, ranging from stretches to hydrotherapy. I showed her how to do fascial work on herself, and how to treat trigger points.
She found relief in joint traction for the wrist and fingers. The symptoms in her neck, ring and little finger were the first to diminish. After a month the swelling and sensation of pain and tightness in her hand were much less. She rarely had numbness and tingling in her thumb, index and middle fingers at night, and was able to return to work.
Gradually, as her symptoms continued to decrease, we added in strengthening exercises for scapular retractors, and then flexors and extensors. At the end
of three months, her grip strength (tested by dynamometer) had improved significantly. When she saw the neurologist for a check-up at the four-month mark, it was decided that unless her symptoms returned, surgery wouldn’t be necessary. Several years later, my client remains free of hand and arm symptoms in her ring and little finger as long as she maintains her self-care stretching regimen. The classic CTS portion of her symptoms did not return.
For me, this was an important reminder of investigating the origin of all reported hand symptoms and not just accepting a diagnosis at face value.
REFERENCES
• Gerard, Janet A., and Steven Kleinfield. 1993. Orthopedic Testing: A Rational Approach to Diagnosis. New York: Churchill Livingston.
• Hertling, Darlene, and Randolph Kessler. 1996. Management of Common Musculoskeletal Disorders, 3rd. Ed. Philadelphia: J.B. Lippincott.
• Kendall, Florence, Elizabeth McCreary, and Patricia Provance. 1993. Muscles, Testing and Function, 4th Ed. Baltimore: Williams and Wilkins.
• Magee, David J. 1997. Orthopedic Physical Assessment. 3rd Ed. Philadelphia: W.B. Saunders Company.
• Schumacher, H. Ralph. 1993. Primer on the Rheumatic Diseases, 10th Ed. Atlanta: Arthritis Foundation.
• Travell, Janet G. and David Simons, 1983. Myofascial Pain and Dysfunction: The Trigger Point Manual. Baltimore: Williams and Wilkins.
Print this page