
Features
Practice
Technique
Essentials of Assessment: Winter 2002
There are many influences on our posture. The first influence is gravity. The overcoming of gravity is the primary determination of the balancing act that the musculature performs to hold us upright. Other influences include occupational or recreational activities.
September 16, 2009 By David A. Zulak MA RMT
There are many influences on our posture. The first influence is gravity. The overcoming of gravity is the primary determination of the balancing act that the musculature performs to hold us upright. Other influences include occupational or recreational activities. Bony structure and the state of the body’s physiology can affect our posture. Pathologies, emotional stressors, and certainly pain all affect our posture. (1) Changes to posture affect our musculature; altering the balance between muscles by making some muscles short and others long.
When the relationship between muscles that are balanced against each other, (agonist and antagonist, flexor and extensor, etc.) becomes imbalanced then posture and function of the body must change, usually for the worse.

|
|
|
|
Kendall says of muscle imbalance: “Weakness permits a position of deformity; shortness creates a position of deformity.” (2)
The imbalance is that one muscle becomes too high in tone and shortens as it tightens. The result is that its balancing musculature often lengthens and becomes weaker.
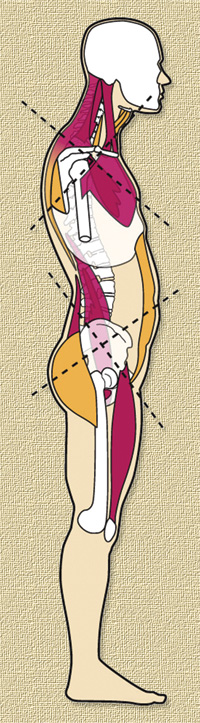
The opposite is also true: If a muscle weakens and lengthens then the opposing muscle becomes short and tight. Janda (3) has shown how this occurs in patterns that have become know as the lower cross syndrome and the upper cross syndrome (see diagram at right).
Janda noticed that the muscles that tighten are the muscles that are responsible for sustaining our posture in both static and dynamic states. Many of these muscles, but not all, that tend to tighten are two joint muscles.
The muscles that tend to go weak and long are referred to as “phasic” muscles. They are muscles that work only to perform specific tasks when called upon, but are not responsible for sustaining our posture.
The changes to posture and function that occur are often the predisposing factors leading to injury or to overuse syndromes. Common examples are headaches, low back pain, rotator cuff strains, thoracic outlet syndromes and patellar femoral pain syndromes.
On the other hand, muscle imbalance can be the result of traumas as the body tries to protect itself through splinting, or as we compensate for temporary losses of function. If the injury persists for more than one or two days the body often adapts to its new posture and function and takes this as now ‘normal’. Though antalgic movement patterns may lessen and disappear the body is often left with changes due to the alterations in muscle balance that have taken place.
The postural changes that occur due to muscle imbalance affect other structures. (4) Compression syndromes that are a result of postural deviations affect neurological, vascular, and lymphatic tissues; creating neurological signs and symptoms, and/or with vascular changes directly affect tissue health and function.
Other structures affected by postural deviations include joints and the mechanical changes that may lead to degenerative joint changes, or to a predisposition to injury to supporting ligaments or musculature.
Visceral organs can undergo stress when changes that affect the abdominal cavity (such as an anterior pelvic tilt) and/or the rib cage are the result of postural deviations. Visceral changes include the tractioning of bile ducts, rotations of organs leading to possible physiologic alterations in function, tractions or compression of sympathetic nerves or ganglia.
Lung capacity and function can be affected by postural deviations to the cervical spine and the ribcage: Scalenes shorten and lift the first two ribs making them insufficient to come into play when axillary capacity for the lungs is required due to increased demand. Changes of the rib cage mechanics can do the same.
Muscle imbalance and the resultant postural deviations are often the primary reason for degenerative joint disease (such as osteoarthritis), especially in the spine, pelvis and lower limbs, and for degenerative disc disease in the spine. There is the obvious situation of changes to the curves of the spine, rotations of limbs, etc.
|
|
|
|
The other more subtle reason is due to what has come to be called the “tensegrity” (5) (tensile/tension integrity) model. It proposes that the spine, for example, should not be looked at as merely column, or a
set of blocks that are stacked one on top of the other with increasing compressive forces accumulating as we go down the vertebrae.
Rather, tensegrity is meant to explain how, when we add the ribs and muscles to the picture, the forces are distributed by the tension in the muscles, and fascia, through their attachments on the ribs and vertebrae in a way that reduces the compressive forces going through the spinal column. (6)
Creating an imbalance in the tension will change the dynamics of tensegrity of the trunk causing exponential stress on some muscles or connective tissue (cables) while others go lax and no longer do their job.
Those taking the strain suffer from tensile overload – tendonitis, shortness, and hypertonicity. Those that are lax suffer atrophy.
We also will have an exponential change in the compressive forces traveling down the spine. Further, these forces are no longer evenly distributed – anterior surfaces of thoracic vertebrae, facet joints in areas of lordosis, uneven stresses on the cartilaginous discs layers, etc.
There is an important palpatory observation we need to keep in mind when investigating the musculature for shortness and excessive length. Muscles are palpated as lax, relaxed, as having normal tone, or as taut.
We often make the common mistake of calling them ‘tight’, but what we are really feeling is tautness. (7) We need to check the length of a muscle before we can say it is tight, because tightness implies a short, even contractured muscle. However muscles can be long and taut. If a muscle is stretched it becomes taut.
If we have confused tautness with tightness we can make the mistake of thinking a lengthened taut muscle is tight and therefore short and proceed to lengthen an already overly long muscle. This could result in making the client’s postural deviations worse.
For example, clients with a forward head and shoulders posture often have an excessive kyphosis: Tight pectoralis and posterior cervical muscles, with weakened and lengthened rhomboids, middle and lower trapezius muscles.
The client often enjoys the mid thoracic area being worked during massage and the therapist often mistakes the tautness of these muscles as tightness and proceeds to relax and lengthen them further.
This may make the client feel temporarily better but, in fact, it only makes their shoulders roll forward more and exaggerate their kyphosis.
We can go beyond the muscles mentioned by Janda and see further implications.
One example: In the upper cross syndrome the long rhomboids allow the serratus anterior to go short.
The connective tissue component shortens as well over time and hence the serratus end up contractured
(that scapulae you cannot lift off or mobilize well).
Further, if you only lengthen the pecs, the SCM and posterior cervical muscles and then strengthen or ‘wake up’ the inhibited rhomboids and lower traps and add tone to the deep neck flexors, those shoulders will not go back if that serratus (along with the latissimus dorsi and teres major) are not lengthened as well.
Oh, the web the body weaves!
Assessment of muscle Balance/Imbalance
• Janda suggests three stages in the assessment of muscular dysfunction (8)
1. postural assessment
2. muscle length
3. evaluation of movement patterns
1) Postural Assessment
We need to do a basic postural assessment of posterior, anterior and lateral views noting where differences from the ‘norm’ appear.
Our focus for the lower body can be on noting anterior and posterior pelvic tilts, (whether bilateral or unilateral), pelvic obliquity, pronation or supination of the feet, varus or valgus knee orientations, and rotations of pelvic, femur and/or tibia.
Our focus for the upper body can be on the carrying angle of the arm, rotations in the parts of the arm, forward head and/or shoulder posture, lordosis of the low back, kyphosis of the thoracic spine and the lordosis of the cervical spine, and, rib cage appearance (flatted, compressed, barrel shaped, etc.). All the while we would be noting muscle bulk and tissue health and changes.
2) Muscle Length (Lower Body)
We can now move to testing the length of the “tonic” or postural muscles, along with a few assesssory or “phasic” muscles.
For the lower body we need to establish the length of the hip flexors.
The primary test for this is the ‘modified’ Thomas Test. This gives us primarily the length of the psoas and of the rectus femoris.
We can also see iliotibial band and tensor fasciae lata shortness with an externally rotated tibia (while the femur is aligned) and possibly an abducted orientation to the leg.
Tightness to the piriformis (and other lateral rotators) can be seen in external rotation of the femur, and this should be confirmed later by palpation.
Janda suggests (9) that we can make these observations while the client is in the Thomas test position: We can check the length of psoas by trying to get 10-15 degrees more of hip extension by overpressure/stretch.
We should be able to stretch the rectus femoris by getting the knee flexed to 100-105 degrees.
If we cannot get 15-20 degrees of hip adduction we should suspect shortness in the tensor fasciae lata and gluteus medius and minimus. If we cannot abduct the leg by 15-20 degrees then we have short hip adductors. The hip adductors could also be checked by FABER’s test.
A straight leg raise can check how much the hamstrings can lengthen. The hamstrings, in the lower cross syndrome are often ‘eccentrically contractured’ – contractured in a lengthened position.
In the lower cross syndrome they are all that is left to prevent even more anterior rotation of the pelvis as the abdominals etc. are not doing their job.
Hence the body has fibroblast spin out collagen fibres to help support the hamstrings in resisting any more lengthening. (Hence, only release or lengthen the hamstrings once all the muscles that are contributing to a lower cross syndrome have been addressed, otherwise you will exacerbate the anterior pelvic tilt.)
Janda further suggests that we check the quadratus lumborum by having the client side lying and have them lift their upper body off the table and hold that position with the straight lower arm.
The greater trochantor needs to remain on the table. The sign for shortness is a strait lumbar spine rather then the normal curve seen. (Note: Mechanical or motion dysfunction between two segments will appear as a straightness between those two segments with excessive motion above or below the dysfunctioning ones.) He feels that this is more accurate than having the client standing or sitting and side bending.
We can check the soleus by a ‘squat test.’ The soleus is short if a person cannot squat without raising the heels off the ground.
Forward flexion of the lumbar spine can best be checked by a standing flexion test. We need to be careful to note that the movement is not coming from the hip only or primarily. The length from S2 to T12 should increase in length from 5 to 8 cm when measured with a cloth tape.
| Notes on Treatments We need to stretch out the tight musculature first before we begin strengthening weak muscles that are being inhibited. Otherwise we only make the syndrome worse. Lengthening tight antagonists can increase the strength of a muscle by This later technique can reciprocally inhibit the previously hypertonic The fascial contracturing would first have to be broken down by |
2. Muscle Length (Upper Body)
Pectoralis length test: Supine. Test in two positions:
Arm at 80 degrees of abduction for the clavicular attachments
of pectoralis major. Arm at 120 degree to test the length of the sternal division of the pectoris major. Normal length is the arm coming level with the table. This will also stress the pectoris minor. Its length is best seen by observation, i.e. by the
shoulders being lifted off the table (protracted).
Forward flexion of the cervical spine: First see the length
of the posterior musculature of the cervical spine by having the client tuck in their chin and then forward flex. They should be able to get within two finger widths of their chest.
To test the strength of the anterior muscles of the cervical spine do in supine: we note weak cervical flexors by the chin jutting forward to initiate action. This may be made clearer with the therapist applying slight resistance on the client’s forehead. Pushup test for the serratus anterior. (Note: Though the serratus anterior can be inhibited with the upper-cross syndrome and protracted scapula it can contracture into a shortened position. Often overlooked and ignored during treatment.)
Latissimus Dorsi and Teres Major: Supine. With lateral
trunk flexion and elbows extended: See if they can forward flex the arm till the arms lay overhead flat on the table with the low back still on the table.
3) Movement Patterns
Janda asks us to note the following movement patterns:
Hip extension: We note by palpation that the gluteus maximus engages weakly and delayed with respect to the hamstrings and especially the erector spinae.
Hip abduction: With the client side lying we suspect weakness of the abductors if we note lateral rotation of the pelvis and femur. This implies that the tensor fasciae lata has “initiated and even dominated the movement.”
The abdominals: We use an abdominal curl to note whether
the hip flexors are dominating the movement.
Check range of motion for shoulder abduction. Have the client do so bilaterally while you palpate the clavicles midway between the sternum and acromium: ensure the clavicle rolls back as the client’s arms go past 90 degrees of abduction and continue to do so till full abduction is reached. (Rolling for a total of approximately 50 degrees. If it will not roll they cannot abduct.)
Pectoralis minor: Ability to retract the scapula with retraction affecting the orientation of the glenoid fossa as well. (i.e., the scapula should not elevate as they retract.)
Endnotes
1) Clinical Biomechanics: Musculoskeletal Actions & Reactions, (1987) Schafer, p.132
2) Kendall, p.184 (See pages 183-185)
3) “Muscles and Motor Control in Low Back Pain: Assessment and Management” Gwendolen A. Jull & Vladimir Janda.
4) See Schafer, pages 132-136, for some of these examples, and for others.
5) A term coined by the inventor and architect Buckminster Fuller (the geodesic dome). A structure that is a mixture of tension through cables attached to material that can resist compression is stronger yet more flexible than a structure made up of only solid material. (Think of the CN Tower).
6) For a discussion of the tensegrity model applied to the body see Anatomy Trains by Thomas W. Myers (2001)
6) Kendall, p.184
7) Jull &Janda, p.263ff.
8) Jull & Janda p.267
Print this page