
Features
Practice
Technique
Essentials of Assessment: Spring 2003
Joint mobilization is one of those wonderful techniques that both helps assess joint impairments and is available as potentially the most beneficial modality to employ in treating joint dysfunctions. This is true whether these dysfunctions or impairments are intrinsic to the joint [ligament or joint adhesions] and/or whether they are due to the shortened surrounding extrinsic supportive structures like connective tissue and muscle.
September 17, 2009 By David A. Zulak MA RMT
Joint mobilization is one of those wonderful techniques that both helps assess joint impairments and is available as potentially the most beneficial modality to employ in treating joint dysfunctions. This is true whether these dysfunctions or impairments are intrinsic to the joint [ligament or joint adhesions] and/or whether they are due to the shortened surrounding extrinsic supportive structures like connective tissue and muscle.
Many massage therapists limit their use of joint mobilization to passive joint movements like ‘rocking and shaking’, sometimes called ‘rhythmic mobilization’. There is so much more to these skills. Joint mobilization techniques are underused or ignored altogether by many MT’s. Its use in passive testing for clarifying the nature of joint dysfunctions cannot be overstated. It is also often forgotten as a useful modality as we all to often focus on muscle, overlooking other soft tissues like joint tissue and their intrinsic structure.
|
|
 |
|
|
|
In order to discuss joint mobilization let’s use its very terms to clarify some of its uses and the understanding it gives therapists concerning joint impairments.1,2,3
“Joint Mobilization” (or sometimes “Joint Manipulation”) is a passive technique employed to mobilize the joint to varying degrees from small oscillations that aid in promoting joint tissue health and/or to cause a reflex effect in the surrounding musculature to relax and drop in tone. On the other hand, it may involve using stretching movements to mobilize a joint so that adhesions are broken down and a fuller range of motion is returned to the joint.
“Physiologic Movements” is the term used to describe the normal voluntary movements of limbs, whether in anatomical planes or through various multiple planes.
“Accessory Movements” are those movements that occur within the joint that enable the joint to go through its range of motion. These are sometimes called “component motions.” For example, for the glenohumeral joint to go through the full range of abduction the humerus must both roll and glide (or slide) inferiorly on the joint surface, not to mention rotate or ‘spin.’ Each of these (roll, glide, spin) is an accessory movement. The client cannot voluntarily do only one of these and not the others. Using passive movement with appropriate stabilizations the therapist can assess the slide movement independently of the other movements. Two other component motions are compression and distraction of joint surfaces.
“Joint play” is used to describe that slight laxity, play or give between conjoining joint surfaces that permits the accessory movements to occur. This term is usually reserved for synovial joints.
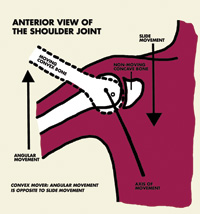
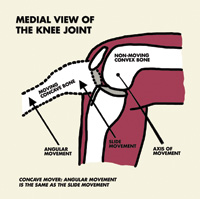
The notorious ‘Concave-Convex Rule’ needs to be understood in order for a therapist to understand (or to figure out for themselves) how to know which way to mobilize the joint to increase the slide. Slide is usually the accessory movement that is lost in the complex mix of movements. Slide needs to be increased in order to increase the range of motion of a joint.
If the concave side of a joint is moving the glide is in the same direction of the physiological movement of the bone (e.g. a proximal phalange moving on a metacarpal, either in flexion or extension). If the convex side is moving the glide is in the opposite direction of the physiological movement. (The abducting shoulder needs the humerus to slide down as the arm goes up.) See illustration on next page. The axis of movement remains in the convex bone regardless of which bone is moving.
The ligaments, along with the fibre directions (or twists) in the fibrous joint capsules, combined with the shape of the joint surfaces, guide or steer the motions that can occur within a joint. Together these elements drive the motion possibilities of the joint. By examining the component motions that occur within a joint, and by noting how well or how poorly these motions occur, we evaluate the health of that guiding structure. Hence, while we are all taught that ligaments support, hold joints together or restrict motions from occurring in specific directions, we often do not spend enough time learning to understand how they guide and steer movements within the joint. In turn we need to link this understanding with how muscles interact with the intrinsic joint structures in also helping to steer movements of joints. This is the missing biomechanical or arthrokinematic information passed over or presented too briefly in anatomy and assessment classes.3
Arthrology definitely needs a lot more attention in massage therapy schools and graduate courses than it is presently given. If we do not understand the biomechanics and component movements of joints
we cannot adequately, (not to say safely!) assess, mobilize or manipulate joints. Nor can we appreciate the role of muscles as more than just movers of joints. The usual solution for a massage therapist when confronted with joint dysfunction is to refer out to chiropractors, and so give some clients away that we should be capable of treating adequately. It literally pays to know your joint ‘mobes.’
As an assessment tool, therefore, joint mobilization gives great depth to our understanding about what can be restricting movement or causing pain for our clients with hypomobility.
To be able to rule in or out the intrinsic structures of the joint as having a primary impact on the client’s impairment is of great value. Not only on how we will further assess the impairment but also on how we will understand the results of our other assessment tests. Is the hypomobility due to muscles high in tone and short in length, or could this be in concert with an intrinsic dysfunction of the joint. Hence our treatment plan will reflect this other dimension of information.
As a mode of treating it helps us reverse hypomobility due to adhesions of joint capsules and ligaments by stretching these structures. Such stretching is used in chronic situations. The clearest example of use is adhesive capsulitis of the glenohumeral joint. The contraindications are principally concerned with acute stage of injury (edema or sprains) or some degenerative disease process.
Small oscillations within the available play of a joint (meaning with no stretch on any structure) can inhibit sensations of pain as well as reduce the tone of muscles that are holding and guarding that injured joint. Further, small amplitude oscillations can reduce the tone of hypertonic or spasming muscles that are crossing a joint even if there is no intrinsic restriction in the joint itself.
These oscillations are also beneficial for general joint health by moving synovial fluid about the joint and so aid in nutrient exchange.1,2,3
Imagine someone with an acute injury to an ankle that then limits knee and hip movements. Applying oscillations to the knee and hip helps to maintain joint health and mobility.
Pain free small oscillations can be used on even the acute joint to aid in the reduction of swelling and pain.
This is without a doubt the most useful technique, along with cold hydrotherapy, for helping the healing of injured or degenerating joints.
Peripheral joint mobilizations are not the whole story.
All joint mobilizations outside of “high velocity, low amplitude” adjustments are available to us.
‘Flat’ joints like the facet joints in the spine tend to slide in the direction of physiological movement.
Facet joints of the spine can often be freed up, just like peripheral joints, either by tractioning or by gliding to the end of range and then gently applying overpressure to break down adhesions.
A useful example of this is when treating restrictions in the lumbar spine. With the client prone flex their knees to 90 degrees and then draw the feet towards you as you stand at their hip. The resulting rotation in the low back opens the lumbar facets.
If they are hypomobile as a group you can ‘tease’ them open by now running the heel of your palm (pisiform) from S1 to L1 just laterally to the spinous processes where you would expect the transverse processes to be. Using the TVPs as levers the facet joints can be mobilized.
I start with light pressure and work with increasing pressure as long as the client remains pain free or has no other adverse or unusual sensations.
If you are treating each facet individually, then position the client as above but rather than running up over the TVPs, landmark and give each sustained pressure for several seconds to several minutes. (The longer the tractioning to open the joint the lighter the pressure should be.) When you finish all the spinous processes should be in a gentle curve if the rotation is held, and all should be aligned strait when you take the rotation away.
Now, as spinal facets can be “stuck” open as well as closed, you can swing the feet to the far side of the table, moving the facets into closure and now sweep from L1 to S1 with the pressure closer to the spinous processes, along the articular processes.
Again, you can treat each individually. In fact, I would go to the other side of the table, bring the legs towards me, and then do a lateral challenge to a spinous process away from me (i.e. push on the lateral side of the spinous process) in order to ensure I was being specific enough.4 Being this specific provides both a good assessment5 and a good treatment.
Add a little contract and relax resistance with the client using only a pound or less of pressure and viola! – Muscle energy technique. Now the tone of the restrictive (holding and guarding) muscles is lessened as the joints are mobilized.
Joint manipulation is a great ‘two in one’ technique in that it allows you to assess and treat the client simultaneously. Our scope of practice really does include soft tissue other than muscle. Incorporating joint tissues and structures into our practice increases our range.
References
- For a great introduction to joint mobilization (and it is often a required book in schools) also with abundant information of the appropriate manipulations for peripheral joints see Therapeutic Exercise: Foundations & Techniques Carolyn Kisner & Lynn Allen Colby, 4th Ed. F.A. Davis 2002; p.216-17ff
- For an excellent text on Joint Mobilization see Manipulating and Mobilization: Extremity and Spinal Techniques by Susan L. Edmond M.P.H., P.T.; Mosby 1993.
- See Hertling, D. & Kessler, R., Management of Common Musculoskeletal Disorders, 3rd Ed., J.B. Lippincott, Philadelphia, 1996. This text, which I have noted often remains wrapped in its plastic until students get to my class, is a valuable resource and has a great introduction to arthrology (Chapter 3) and introduction to joint mobilization technique (p.119-127). Further, it has great descriptions and illustrations or photos of joint mobilizations for all major joints of the body including the spine, making it a great companion to Kisner & Colby’s book.
- Note, you are opening the joint on the side you are on, and closing the other side. Hence you can work one side using the TVPs and then do the lateral challenge, with the legs towards you with both techniques. You are then assisting opening one side as you assist closing the other, which has to happen anyway. The only way a facet on the spin can fully open is if its contralateral joint can fully close.
- The first technique treats a group dysfunction where there is a loss of hypomobility throughout the lumbar spine. The specific technique is where one pinous processes is out of alignment suggesting a single joint dysfunction. That either one side is not opening or the lateral side is not closing. Personally, I treat both just to ensure that all structures and muscles are realigned and integrated.
David A. Zulak has been teaching clinical assessment since 1995. Presently, he is the director of massage therapy for an Ontario private vocational school that has several campuses. He is co-ordinator for the Hamilton campus and, of course, teaches assessment.
Print this page