
Features
Patient Care
Practice
The lumbar spine: Common postures and how they affect the lower back
Common postures and how they affect the lower back
(For more details on types of postures and the impairments they present with, see: Janda & Jull 1987; Kendall et al. 2005; Magee 2014.)
February 5, 2019 By David Zulak
 This text aims to bring together a range of examination and assessment techniques only otherwise found in a variety of different places. Excerpted from Clinical Assessment for Massage Therapy
This text aims to bring together a range of examination and assessment techniques only otherwise found in a variety of different places. Excerpted from Clinical Assessment for Massage TherapyIn the normal posture (Fig. 12.8) the ear sits roughly over the shoulder, the shoulder sits over the trochanter and the gravity line runs just behind the patella and just in front of the malleoli. The spine has its proper elongated S-shape that provides a spring to cushion the joints and structures of the spine. The line of gravity (plumb line) runs through the body of vertebra L3.
In sway back (forward hip) posture (Figure 12.9), sway refers to the tendency of a person with this posture to sway back and forth (i.e., anteriorly and posteriorly). The reason for this is that with the hips thrust forward, their weight will shift onto the toes and this easily creates a feeling of imbalance so the musculature of the legs and hips will alternate in tension, causing the person to sway back to front as they remain perched on their toes (Kendall et al. 2005). The lumbar spine is extended (hyperlordotic) at the lowest lumbar vertebrae, which are sitting on posteriorly rotated hips. The hip joint is in extension, as are the knees. (The thoracic kyphosis and cervical lordosis are also exaggerated.) The first one or two lumbar vertebrae and lower thoracic vertebrae are often flattened and resist motion. This adds to the compressive force on the lowest hyperextended lumbars.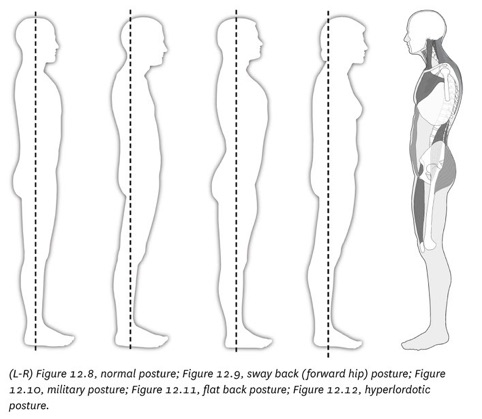
Muscles creating sway back posture:
- Tight and hypertonic muscles: lumbar erectors, quadratus lumborum; hamstrings and gluteus maximus (for the knees: vastus medialis, vastus lateralis, vastus intermedius).
- Weak and inhibited muscles: abdominals, except for internal oblique which may be hypertonic, iliopsoas, rectus femoris.
The military posture (Figure 12.10) is named for the classic “head up, stomach in, and chest out” position of a soldier at attention. It requires the person to extend their low back (increasing lumbar lordosis) while lengthening or flattening the thoracic kyphosis as the shoulders are retracted. Often the chin is lifted, extending the upper cervical spine. Note that the line of gravity runs slightly behind L3’s vertebral body.
Muscles creating the military posture:
The low back and mid-back erectors are short and tense, abdominals are tense, rhomboids and lower trapezius are short and tense. The suboccipitals are short and tense, along with the scalenes (holding the first two ribs up). The pectoral muscles are also short and tense (lifting the ribs and sternum while lowering the clavicle onto the ribs underneath it).
In the flat back posture (Figure 12.11) the lumbar spine curve is decreased/ flattened. As a result, the body compensates for this by throwing the head forward (upper thoracic hyperkyphosis and upper cervical hyperlordosis).
Often, the whole body tilts forward which results in the toes grabbing the ground and the toe flexors, therefore contributing to a pes cavus (high arch) in the foot.
As a result of the at back posture, the pelvis-lumbar complex has:
- Lumbar spine flexed, stretched low back erectors
- Posterior pelvic tilt with extension of hip joint, tight, short hamstrings, short abdominals and lengthened rectus femoris and iliopsoas.
Hyperlordotic posture (lower cross syndrome)
The hyperlordotic posture (Figure 12.12) is associated with a bilateral anterior pelvic tilt, which is a common muscle imbalance found in the clinical setting.
Tight and facilitated muscles:
- Lumbar erectors, QL, iliopsoas, piriformis, rectus femoris, TFL, thigh adductors.
- Taut hamstrings (lengthened but hypertonic): the hamstrings are stretched by being a muscle group holding the pelvis from rotating further anteriorly (along with gluteous medius) and, over time, contracture to this length. Because of this contracturing, they will appear short (loss of extensibility) when tested for length.
Weak and inhibited muscles:
- Rectus abdominis, transversus abdominis, gluteals, vastus medialis and lateralis of the quadriceps.
Lumbar curves and L3: The source of many impairements and dysfunction within the lumbar spine
The lumbar spine’s normal lordosis (anterior curve) is meant to act as a spring to cushion the forces coming from below (as when walking or running) or from above (as in upper body movements and carrying or lifting). This springiness comes from the shock-absorbing qualities of the intervertebral discs (IVDs). This works well when the spine is generally in a neutral position. In neutral, the plumb line, or line of gravity, runs through the vertebral body of L3, which is also the apex of the normal lumbar lordosis (Bogduk 2012; Mitchell 2001).
However, in most of the postural variations (from neutral), the lumbar curve is held out of line, or repositioned with respect to the line of gravity. This means that the direction of forces on L3 (and the rest of the lumbar spine’s vertebrae and IVDs), are altered. While the lumbar spine is accepting and capable of handling such repositioning for brief moments, the spine is not capable of handling this for long periods of time. Changing the lines of force and tension, etc., inevitably will result in changes to structure and function of the tissues of the spine.
The IVDs, the facet joints, the bony structures and the ligaments are all put under long-term tensile and compressive stresses that will inevitably affect those structures physiologically and structurally. Changes to the orientation (or structure) of the lumbar spine’s curvature will inevitably change how it functions. Changing how the spine functions for extended periods of time will in turn begin to change the very structure of each of the components listed above. Such changes are the primary causes of degenerative disc disease (DDD; disc degeneration, herniation, vertebral body osteophyte formations, etc.) and degenerative joint disease (DJD; e.g., facet joint osteophyte formations, ligamentous stretching or shortening, synovial joint surface osteoarthritic changes, etc.). Most of these changes, after prolonged postural deviation, are permanent (or only minimally reversible or repairable), even if the normal curve is returned to neutral.
Some examples of lumbar curve impairments and their effects include:
- During hyperlordosis, L3 is shifted in front of the line of gravity. The more L3 moves forward of the gravity line (as in excessive hyperlordosis, e.g., in a sway back), the greater are these excessive forces on the posterior portion of the IVD, resulting in degeneration (cracking and tearing) of the annular fibers. In fact, the nucleus pulposus, which was centered under the lines of force running through L3 (by being slightly posterior within lumbar IVDs), is now being shifted forward of the line of gravity, etc. It now can actually become a fulcrum increasing the amount of compressive forces in the posterior portion of the IVD and the tensile (stretching) forces in the anterior portion of the IVD, much in the same way as shifting more weight to one side of a seesaw (teeter-totter). Osteophytes will begin to form anteriorly in order to try to hold or reinforce the stretching annular fibers, and also posteriorly to reinforce the posterior annular fibers from being crushed and broken down.
- Further, this shift of force or weight may make the facet joints become weight-bearing. This will speed up osteoarthritic changes in these joints. The pars articularis will also receive excessive force and may crack. Ligaments around the facet joint become shortened and so can no longer appropriately guide the movements of the facet joints nor properly stabilize the joints at their end-range. This permits excessive side-bending and rotation within the lumbar spine. All of this can also threaten impingement of nerve roots by decreasing the size of the neural foramen.
- A scoliosis (rotoscoliosis) is a lateral curve; a side-bending and rotation in the spine. In the lumbar spine, L3 shifts away from the side to which the spine is bent. As a sustained orientation (posture) of the spine, changes (as in hyperlordosis) to the forces running through the lumbar spine (from above and below) will occur. However, with a scoliosis, the compression happens on the concave side, and the increased tensile forces happen on the convex side. With the addition of rotation (that happens in a scoliosis) the compressive forces are increased within both the disc and the facet joints on the concave side.
- During hypolordosis, L3 may remain somewhat in the line of gravity. However, the flatness of the lumbar spine (from its flexed position, relative to the pelvis) is what changes the lines of force running through the IVD in this case. Now compression occurs in the anterior portion of the disc and tensile in the posterior portion of the disc. The facet joints are gapped excessively, and can no longer momentarily help with weight- bearing during extension of the lumbar spine, nor appropriately guide motions within each spinal motion segment. Stretch (tensile) forces occur to the posterior ligaments and facet joint capsules. e stretch of ligaments around the facet joints will cause these ligaments and joint capsules to undergo excessive tensile force on flexion, rotation, and side-bending: either as individual motions, or especially during a combined motion of all three. Thus making it easier to strain and tear these ligaments, especially if the person is carrying or lifting something.
Due to these changes in the curve of the lumbar spine, we can clearly see how the possibility of injury to the structures of the vertebrae will increase as the deviation of L3 (and all vertebrae) increases from a neutral position. These postural deviations may well play a part in the predisposing factors (or even causes) of most lumbar spine impairments and dysfunctions.
Print this page