
Features
Continuing Education
Education
Spinal Motions
I want to talk about the living spine. Though a very broad topic, my purpose here is to provide a general overall picture of the living spine, i.e., the spine in motion. I want to describe some of the ways in which the spine functions according to the nature of its structure, and also show how the structure and function can become impaired or dysfunctional. What follows must be, by necessity, general in nature. Further, I will skip the pathological changes that may occur over time, or those due to disease processes.
August 20, 2010 By David A. Zulak MA RMT
|
I want to talk about the living spine. Though a very broad topic, my purpose here is to provide a general overall picture of the living spine, i.e., the spine in motion. I want to describe some of the ways in which the spine functions according to the nature of its structure, and also show how the structure and function can become impaired or dysfunctional. What follows must be, by necessity, general in nature. Further, I will skip the pathological changes that may occur over time, or those due to disease processes.
The usefulness of looking at the spine in this way, even though it is removed from its environment in the body, is that it helps the therapist imagine, or visualize, those structures intrinsic to the spine and how they function. I call this type of exercise thinking anatomy, thinking through the implications of the structure and function of the musculoskeletal system. Structure (anatomy) permits and informs function, and function (physiology) shapes structure. In this way we can envision how the body seeks balance, successfully or unsuccessfully.
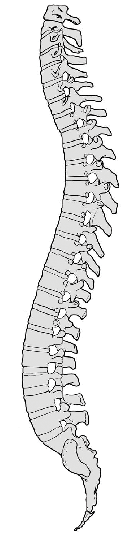
The spine acts as a spring or shock absorber for the trunk and head. Looking at the spine in profile, we see familiar curves. These curves allow the spine to act as an S-spring. Pressure from above or below compresses the structure, but not in ways exactly like the loading on a solid column. Rather, the curves become exaggerated, absorbing stress from the load, while the elasticity inherent in it (via intervertebral discs, ligaments, muscles, etc.) pushes back. When the load is removed, the spine can lift itself back into its original shape, even without muscular action. This assumes the load was not so great as to deform inert tissue or injure and impair muscle function.
INTERVERTEBRAL DISCS
Some of this absorption of forces comes from the intervertebral discs (IVDs).
The IVD is a polyaxial joint. It can accommodate any direction of motion, including shear forces, as well as compression and decompression.
Similar to a gel, the ball-shaped nucleus pulposus at the interior of the IVD is uncompressible; it cannot lose volume. When under pressure it pushes back. It acts as a self-righting mechanism for the spine, and this ability also allows the annular fibres around it (which can deform) to re-inflate. Further, the nucleus, because it is uncompressible, acts as the axis of motion between vertebrae – as a swivel-type joint. It remains gel-like until middle age, when it then becomes fibrosed. When this happens, it loses its capacity to recoil under pressure, and so the cartilaginous layers within it can more easily lose their height.
When under pressure, the annular fibres, because they are cartilaginous, can lose water and can therefore be compressed or change shape. This compressibility provides the give within the spine, so that it can work as a shock absorber that helps accommodate the compressive forces exerted on the disc. Therefore, the fibrous portion of the IVD, as compressible, can have its shape altered, when under stress. When the load or stress is removed, these annular fibres re-absorb water, re-inflating. The principle motor driving this re-inflation is the nucleus pulposus. However, if the layers are put continually or forcibly under stress, their integrity can begin to break down.
Constant, or frequently recurring, compression or stress will prevent the annular fibres from taking back their water, leaving them dry and brittle. Then the gel-state nucleus itself will flatten and by necessity, it will begin to push its way outward through the cracks and breaks in the annular fibres and force the layers in front of it to bulge, or herniate.
THE IVD AT VARIOUS SPINAL LEVELS
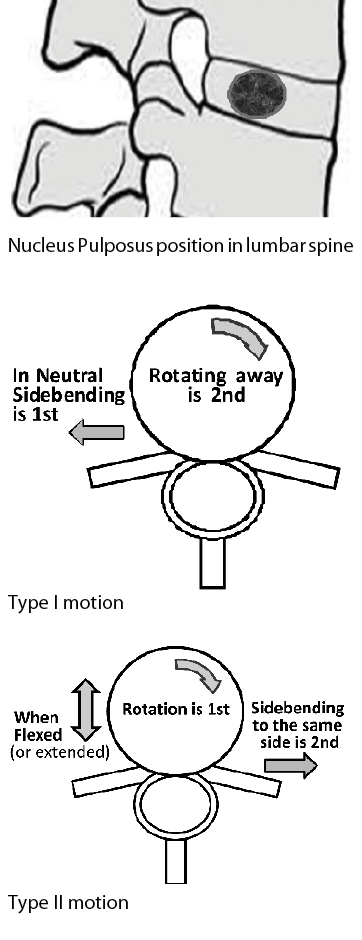
In the lumbar spine, the nucleus is not in the centre of the disc, but is positioned slightly posterior in order to better accommodate the compressive force when the spine is in neutral. In other words, because the lumbar anterior (lordotic) curve puts more mechanical stress on the posterior portion of the disc, the nucleus, being slightly posterior to centre, is better able to provide support.
Therefore, as the lumbar curve exaggerates under load, the posterior-positioned nucleus provides protective support. As long as its integrity holds, the nucleus’ gel-state keeps it uncompressible, so it pushes back, or recoils, and because of this, it can act as a self-righting mechanism. It helps the spine (bone, annular fibres, ligaments, muscles) return to normal shape once the load or mechanical stress is removed, and therefore helps restore its original form.
However, with flexion of the lumbar spine, the compression of the anterior portion of the disc pushes the nucleus even more posteriorly. If the posterior cartilaginous layers are losing their integrity, the nucleus will begin to shift even more posteriorly, causing the weakened layers to bulge, or herniate. The posterior longitudinal ligament (which is quite narrow at the lumbar spine) often helps sustain the integrity of the most posterior fibres of the disc, and so the bulging nucleus often rolls out around this ligament and moves to the side, moving in a posterior lateral direction. This puts it on a collision course with the neural foramen and the spinal nerve at that level.
In the cervical spine, C2 to C7, the nucleus pulposus is also slightly posterior within the IVD, and therefore functions, or dysfunctions, much like the lumbar spine.
The thoracic vertebrae have their nucleus pulposus more centred within the IVD. The lowest thoracic vertebrae, being slightly extended can have the nucleus slightly posterior; the flexed vertebrae have it more centred.
|
BEYOND FLEXION AND EXTENSION
We have talked mostly about flexing and extending portions of the spine. Side-bending functions much in the same way, with the nucleus acting as an axis over which side-flexion occurs. These three motions, of course, do not only move as a teeter-totter does; there is, in addition, some shearing occurring as the vertebra above slides in the direction of flexing, extending, or side-bending. This shearing action can be more stressful to the annular fibres than compression is all on its own.
However, rotation is even more stressful on the IVD’s annular fibres. As the layers of annular fibres run (in general) in alternating diagonal directions, the stress/tension running through the fibres during rotation will be resisted by some, while others are actually made lax. With fewer fibres resisting the forces, they are more likely to break down. Further, rotation also pulls the vertebral bodies closer together. This also reduces their ability to be shock absorbers.
FACET JOINTS
Facet (zygapophyseal) joints are meant to be slightly gapped when the spine is in neutral, or, as some say, the facet joints idle – as with the motor of a car idling – are not engaged or in use, but ready to be used. This occurs the closer the curves of the spine are to being ideal. The structures involved in facet joints (bone, articular cartilage, synovial fluid, joint capsules, ligaments and muscle) all contribute to the weight-bearing ability through the area; yet, the articular surfaces can remain gapped. The weight is distributed throughout the structure, where even the fluid in the joint can hold the joint surfaces apart, with the fluid playing a supporting role as forces move through the joint structures.
However, as the curves exaggerate, the lordotic curves (cervical and lumbar) go into extension and the facet joint surfaces approximate and become weight bearing. These stresses going into the articular cartilage, similar to the cartilaginous annular fibres, lose fluid – it is literally squished out of them. This fluid mixes with the free synovial fluid within the capsule, making the capsule balloon, which still helps the joint, as a whole, resist the forces that are pressing through the bony facet process. However, the internal pressure of the fluid in this weight-bearing situation will stress the synovial and fibrous capsules and prevent nutrients from entering the synovial cavity.
Therefore, the longer this hyperlordosis persists, or the more extreme and forceful the extension: 1) the more quickly their articular surfaces will begin to break down and suffer other osteoarthritic changes; 2) the more likely it is for an injury to the capsules to occur; 3) the more likely it is for injury to occur to the intrinsic spinal ligaments and (fourth layer) musculature, with some overstretched and some left shortened, and 4) the poorer the nutrition will be within the joint.
Now, when the spine moves from neutral, into extension, sidebending/flexing, and rotating, the facet surfaces not only compress but also are going to glide one over the other. This glide or skating also stretches the capsules, and will lengthen some supportive joint tissues, while making others lax. Flexing the spine gaps the joints but generally stretches most of the facet joint tissues.
Therefore, any of these motions (or an undue load) done to the extreme are going to strain and tear tissue. Further, combinations of these motions will exaggerate those forces straining the tissues.
SPINAL MOTIONS
Next, let us examine what are commonly referred to as Fryette’s rules of spinal motion. The first two were formulated by Harrison Fryette, DO, while a third was added by C.R. Nelson, DO. They also have been call laws or principles. I like to use the term rules, as they really should be taken as rules of thumb. They are informative about how the spine can move, but, as is common with many living things, the spine does sometimes seem unaware of these rules or chooses to ignore them.
We must keep in mind that every individual person’s spine is itself individual and unique. No two facet joints are absolutely identical from one person to another, nor are any individual’s two facet joints in their spine exactly identical. They all have at least one small, possibly trivial, unique feature. Some can be shaped quite differently and so function differently, to various degrees. Even the adjoining facet joint surfaces may differ in shape (e.g., one may have a slightly convex surface while its partner may be basically flat), size or even orientation, from one to another.
Before we proceed, we need a couple of definitions and observations:
Motion Segment
A motion segment of the spine is defined as two adjacent vertebrae and all the joints between them. There can be group or segmental motions in the spine, which are clarified in Fryette’s rules of spinal movements. Those rules were meant to apply specifically to both the thoracic and lumbar spine, but not the cervical.
A couple of observations:
Spinal movements are coupled. This means that any motion of the spine impacts on any other motion and, further, that some motions generally accompany one another. With respect to the last point, it has been proposed that side-bending and rotation are always coupled in the spine.
The motions are named from the perspective of the vertebra above, with reference to the one below. Therefore, to say that a vertebra is side-bent and rotated is to say that relative to the vertebra below, the vertebra above is side-bent and rotated.
FRYETTE’S RULES OF SPINAL MOTIONS
These rules have been shown to be especially valid for the lumbar spine.
Fryette’s first rule of spinal movements: When moving from neutral, the spine side-bends first and then rotates in the opposite direction.
Comments
Neutral, here, means the spine is neither flexed nor extended. Side-bending occurs in the frontal or coronal plane. Rotation happens in the transverse plane. When speaking of motions in neutral, side-bending occurs before rotation.
Kapanji says the following, to explain how this coupled movement in opposite directions occurs:
“This automatic rotation of the vertebrae … [When side-bending/lateral flexion occurs] … depends on two mechanisms – compression of intervertebral discs and the stretching of ligaments. The effect of disc compression is easily displayed on a simple mechanical model … If the model is flexed to one side, contralateral rotation of the vertebrae is shown by the displacement of the various segments off the central line. Lateral flexion increases the internal pressure of the disc on the side of movement; as the disc is wedge-shaped its compressed substance tends to escape toward the zone of lower pressure, to rotation, i.e., contralaterally … Conversely, lateral flexion stretches the contralateral ligaments, which tend to move toward the mid-line so as to minimize their lengths … It is remarkable that these two processes are synergistic and in their own way contribute to rotation of the vertebrae.” (Kapanji, vol. 3)
. Fryette’s second rule of spinal movements: When the spine is non-neutral – when in flexion, or extension – rotation happens first, and then side-bending, both in the same direction.
Comments
When the spine is working normally in flexion or extension, rotation precedes side-bending.
Impairments, when they do occur, are likely if the order of vertebral motion is not synchronized.
For example, if the spine is first in neutral and the client side-bends and rotates, and then flexes or extends, the chances of an impairment or dysfunction increase substantially. Knowing the order of movements that produced the client’s injury helps the therapist understand how the client became lesioned. This information can only be obtained from taking a thorough case history.
Fryette’s third rule of spinal movements: Introducing motion to a vertebral joint in one plane, automatically reduces its mobility in the other two planes.
Comments
This rule is fairly self-evident. It is important, however, in understanding how injuries occur. Again, if the client’s spine is moved following the second rule as the vertebrae are flexed, some degree of motion is no longer available for side-bending and rotation. If, however, the person moves the spine into extremes in any of the three planes, that also greatly increases the chances of injury occurring. If the IVD and facet joints are driven too far, then injuries to the joint structures themselves and/or to the intrinsic muscles of the spine are likely to occur.
UNDERSTANDING DYSFUNCTIONS AND INJURIES
The first rule is often referred to as Type I motion. Type I dysfunctions usually occur as a group (as in a scoliosis, for example). Therefore, they are referred to as a group or neutral dysfunction, where a number of vertebrae side-bend in one direction and rotate in the opposite. A functional scoliosis means that the scoliosis does not disappear when the client flexes or extends the spine. The vertebrae remain rotated and side-bent. However, in a bony (or pathological) scoliosis the vertebrae can be rotated and side-bent either to opposite sides or to the same side; they will not be following Fryette’s rules.
The second rule is Type II motion. Type II dysfunctions occur most often when the spine is already flexed or extended, and then, side-bending and rotation are added. They usually occur in isolation, in a single segment strain, with lifting and twisting as an example. In other words, they are segmental dysfunctions, generally not in several segments in a row (as a group). However, it is quite possible to have several segments dysfunction, one on top of the other, but each should be treated as an individual motion segment. Again, this will help us understand how to test for these types of lesions, and interpret the results of such testing.
Note that, when the spine seems in neutral, if the person has hyperlordosis or hyperkyphosis, or excessive or flattened curves, that portion of the spine is not in neutral and will function as Type II motion, leading to Type II impairments. So, for example, if a client with a lumbar lordosis due to an anterior pelvic tilt, now rotates or sidebends, the joints involved will follow the second rule (Type II motion) rather than the first rule (Type I motion).
CONSIDERATIONS
Of special note: The spine is a continuum. Though we refer to portions of it as the lumbar, thoracic and cervical spine, many structures undergo gradated changes as we progress up the spine from the sacrum to the occiput. Of course, it is true that there are transition points, predominately where the ribs come into play, namely, the cervicothoracic and thoracolumbar junctions. (We are ignoring the lumbosacral and occipital-atlantal junctions, as we are removing the spine from its context of the body as a whole.) The ribs have real impact, but we will get to that later.
The point is that the rules apply fairly consistently to the lumbar spine, and up into the lower thoracic spine. However, as the facet joints slowly, but progressively, change their orientation as they move up or down the spine, and as we move into the upper half of the thoracic spine, these rules are going to become less consistent. At a certain point, they will no longer apply to the cervical spine at all. Gradation in spinal structure (shape) results in a gradation of function, and a gradation of how predictive these rules of Fryette’s are.
The cervical spine, from C2 to C3, tends to move with side-bending and rotation occurring to the same side, either in neutral or when the cervical spine is flexed or extended. This is due to the orientation of the facet joint surfaces. However, these vertebrae can be made to move opposite to each other under special circumstances. Hence, Fryette’s rules do not apply to them. Further, the unique shapes of C1 and C2 mean they move in their own unique ways. Therefore, structure informs their function, and vice versa.
DO ALL SPINAL LESIONS OCCUR IN THESE WAYS?
No.
Lesions, by nature, may show patterns, but unusual traumas, severe blows or an unusual structuring or shape to the vertebrae can result in atypical patterns. The rules of spinal movement are meant to help explain common clinical findings. However, because everyone is unique, joint shapes differ from person to person. Any lesion may present as unique. You may, on a rare occasion, find a group dysfunction where the lumbar or lower thoracic vertebrae seem rotated and side-bent to the same side, for example. Alternatively, a segmental dysfunction could have the motion segment rotating and side-bending in opposite directions. After all, lesions are lesions because things have gone wrong! Lesions, by definition, break the rules of normal structure and biomechanics. The joints in the spine can be forced into moving (functioning) in ways that do not conform to their shape (structure). Thus, we need to know how to palpate accurately and test the joints of the spine, and, more importantly, not make assumptions about how things should be and, thus, forgo the testing. We need to be open-minded enough to be prepared to find the unexpected.
WEIGHT BEARING AND THE SPINE
Let us consider how the spine contributes to holding the body upright – how it bears the weight of the trunk, head and upper limbs.
Often the spine is still thought of, or described as, a column (hence the classic name spinal column), that works mechanically like a column, supporting all this weight. However, this is no longer considered an appropriate model.
This is where one of the many important jobs the ribs perform comes into play. Rather than only transferring weight, and other stresses, onto the spine, the ribs can distribute a lot of the weight of the upper body outward, to the body wall.
This transfer of weight and forces outward is referred to as the concept of tensegrity. Tensegrity is a term coined by the architect, engineer and scientist R. Buckminster Fuller, who was the original designer of the geodesic dome. He said his inspiration for that design came from the structures within the living cell, or its cytoskeleton. The term comes from contracting the words tensional integrity: This describes the forces at work in a structure that is formed by a network of compressive, rigid elements interconnected through tensile or elastic elements, which give the structure its overall integrity. Due to the elastic property of the interconnections, when one element of the tensegrity structure is shifted (moved and/or loaded), this shift is spread throughout the whole structure. All the other elements shift as well, adapting and compensating by morphing into a new configuration. By yielding in this way to these shifts, such a structure is more accepting of the forces or loads applied, and will not break.
In this way, the ribs, and all the other tissues and structures of the spine working together, disperse stresses and strains that would cause them to snap if they were a rigid structure. Therefore, the ribs also help the body absorb the forces of walking, running, weight bearing, reaching, pulling, etc. This is in addition to their duties of being the bellows for breathing and fluid movement (as part of circulatory system, especially for venous and lymph flow through the trunk). The qualities of tensegrity also help the ribs, and their related tissues, be even more effective in protecting the organs within the trunk.
By looking at the spine in this way, by seeing its function as guided by its structure, and how its function can shape structure, the therapist is better equipped to understand how the spine works and how it gets into trouble. We can only see this way if we are looking at the spine as a living, changing, adapting system.
David A. Zulak has been a registered massage therapist in Ontario, Canada since 1994, and has been a teacher since 1996. His focus is anatomy, treatments, techniques and, of course, orthopaedic assessment skills. David has been an instructor, and director at several schools. He has written a complete 2200-hour massage therapy program that is used in several schools. David can be reached at dzulak@mountaincable.net.
Print this page