
Features
Practice
Technique
The Story of Fascia
Fascia – the soft-tissue component of connective tissue – weaves its way throughout the body, enveloping, investing and supporting various musculoskeletal elements.
August 4, 2011 By Cathy Ryan
Fascia – the soft-tissue component of connective tissue – weaves its way throughout the body, enveloping, investing and supporting various musculoskeletal elements.
Fascia is highly variable in its presentation (i.e., histological components, fibre ratios and arrangement, and innervations) and fascia’s presentation is determined by its role or function – in turn, the demands placed upon fascia will influence its presentation.
 |
Recent research has identified that fascia is densely populated with nerve receptors. Such elements provide fascia with the ability to perceive and respond to stimuli – including stimuli in the form of pain, proprioception and manual therapy!
Traditionally, among the various tissues involved in musculoskeletal dynamics, fascia has received comparatively little scientific attention. Given fascia’s pervasiveness and multi-tasking capabilities it is that much more disconcerting that fascial involvement in musculoskeletal pain and dysfunction has gone largely unnoticed by the conventional health-care community.
This lack of consideration given to fascia could explain why some individuals do not fully resolve their “soft tissue” pain and dysfunction following a whiplash or a work-related back injury; why some individuals do not resolve a muscle strain injury in the widely accepted time frames; or why an individual is susceptible to subsequent re-injury.
Many are working toward change in this arena. The International Fascia Research Congress (FRC) is a continuing series of conferences dedicated to the emerging field of fascia studies.
One standout at the first FRC (Boston 2007) was the work of Luigi Stecco, PT, who formulated and refined his Fascial Manipulation approach over 30-plus years of clinical experience. Dr. Stecco and his colleagues are now recognized as major contributors to the world of fascia research and fascial manipulation therapy.
Physiotherapist Julie Ann Day has been an integral part of the “Stecco collaborative” since 1999; she has been one of the authorized instructors of Fascial Manipulation – The Stecco Method since 2002, and is also the translator of Fascial Manipulation for Musculoskeletal Pain and Fascial Manipulation – The Practical Part (English editions, 2004 and 2009). Originally from South Australia, she completed her diploma in 1977 and has been living and working in Italy since 1984, mostly in the field of orthopedics and connective tissue massage. Day is a founding member of the Fascial Manipulation Association (AMF). She has taught internationally and was part of the group that won the best poster award at the first FRC, held at Harvard in 2007.
In the following interview with Day, we will explore the nature of fascia and why it should be considered when treating issues presenting with musculoskeletal pain and dysfunction.
 |
|
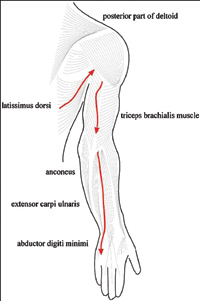
| One myofascial sequence in the upper limb.
|
Massage Therapy Canada: Research findings noted by the Stecco collaborative identified some key regional differences in fascia’s presentation; in particular, the trunk and limbs. Can you describe for us the biomechanical significance of these variations in presentation?
Julie Ann Day: First of all, we need to distinguish between the superficial fascia and the deep fascia.
The superficial fascia is a membranous layer lying within the hypodermis. The hypodermis is involved in the gliding of skin on underlying structures; thermoregulation; metabolic exchange; and the passage of nerves, blood and lymphatic vessels.
The deep fascia surrounds muscles and has a more mechanical function of force transmission as well as a possible proprioceptive role.
Fascial anatomy studies have shown that the deep fascial layer in the trunk is quite different, both morphologically and functionally, from that of the limbs. Generally, apart from the thoracolumbar region, trunk fascia is thinner (approximately 300 millimetres). The large superficial muscles of the trunk region (e.g., pectoralis major, latissimus dorsi and trapezius) have developed within the superficial lamina of the deep fascia, and are not separable from the same. The fascia adheres to these muscles via numerous intramuscular fibrous septa. Many muscular fibres are inserted into both sides of these septa and into the fascia itself, which provides additional insertions for these fibres. In the embryo, these muscles originate as part of the limb muscles, then they extend towards the midline of the trunk. Migration of limb muscles into the trunk forms an additional myofascial layer with respect to underlying muscular planes. This ensures functional continuity between limbs and trunk, including myofascial connections between the upper and lower limbs, and the two upper limbs. This firm relationship between trunk fascia and muscles allows for fine orientation of the vectorial forces created by the activation of the muscles: different portions of these muscles are activated according to the degree of movement, modulating transmission of tension more effectively.
The deep fascia in the limbs is a relatively autonomous structure with respect to the underlying muscular plane. It is much thicker (0.5 -1.8 millimetres), with multiple layers of parallel collagen fibre bundles, each layer oriented in a different direction, and significantly fewer elastic fibres. It is easily separable from the underlying muscles due to the presence of the epimysium, which permits the muscles to slide independently from the overlying deep fascia. A thin layer of loose connective tissue between deep fascia and epimysium facilitates sliding between fascia and the muscular planes. The deep fascia in limbs perceives contractions of the muscle it surrounds due to some myofascial expansions that the muscles extend to the fascia and a few muscle fibres that insert directly onto its inner surface. We can say that limb fascia is less adaptable than trunk fascia but it is ideal for the transmission of force along limbs, so it is suited to the function required of our limbs.
 |
|
| Julie Ann Day is a physiotherapist working with Dr. Luigi Stecco. |
MTC: It is becoming more evident that that fascia displays essentially two distinct functions: it separates, allowing for slide and glide; and it connects, augmenting the transfer of forces and providing stability.
With these basic functions in mind, can you summarize the Fascial Manipulation/Biomechanical Model’s perspective that identifies fascia’s role as a unifying, connecting and co-ordinating element?
JD: The body is a complex system made up of interacting subsystems. We require interpretative models that simplify the complexity. Stecco’s biomechanical model is an interpretation of one of the body’s subsystems, the fascial system. It essentially shifts our focus from muscles with origins and tendinous insertions moving bones, to motor units, activating groups of muscle fibres, united by fascia that bring about movement. It suggests that deep muscular fascia could act as a co-ordinating component for motor units grouped together into functional units and that it unites these functional units to form myofascial sequences.
In synthesis, Stecco divides the body into 14 segments. Six myofascial units move and co-ordinate each body segment. A single myofascial unit (MFU) includes motor units innervating and activating monoarticular and biarticular muscle fibres, the deep fascia that unites these fibres together, and the joint that they move when the muscle fibres contract. MFUs can be considered as the functional building blocks of the myofascial system.
Stecco has identified key areas of the deep fascia, called Centres of Co-ordination, where the tensional forces of each MFU coincide. If the deep fascia in these areas is densified, and not sliding, then the MFU will be dysfunctional.
Biarticular muscles link unidirectional MFUs to form myofascial sequences. A myofascial sequence is considered to monitor movement of several segments in one direction on one plane. While deep fascia derivatives (endo, peri, and epimysium) unite the muscle fibres of single MFUs, fascial anatomy studies have also identified muscle fibres that insert directly onto the inner surface of deep fascia and myotendinous expansions that form bridges between adjacent body segments.
The intricate architecture of deep fascia corresponds to precise motor directions and is intimately involved in musculoskeletal function. The premise is that if manual work can restore gliding to the deep fascia in these key areas then it can influence poor muscle recruitment, myofascial force transmission, faulty movement and pain avoidance patterns.
A few significant resources for fascia information
|
MTC: What is known thus far about the impact of trauma/injury on fascia?
JD: Further studies will be necessary to better clarify the possible alterations of the fasciae in pathological conditions. Different authors claim that trauma/injury can alter properties of the extracellular matrix due to neurophysiological influences, with water loss in the tissue influencing collagen fibre bundle formation and orientation. Others implicate changes in fibroblasts with their transformation into myofibroblasts. Reduced gliding between layers of collagen fibre bundles within the deep fascia could result in an alteration of the mechanical properties of the fascia.
MTC: Can you explain for us the impact of injured fascia on the neural components (fibres and receptors) and the subsequent impact on biomechanical function?
JD: In superficial fascia, we can find free nerve endings: Pacinian and Ruffini corpuscles.
Deep fascia is highly innervated with free and encapsulated nerve endings, such as Ruffini, Golgi-Mazzoni and Pacinian corpuscles. Density of innervation varies according to location, with higher density found in retinacula compared to deep fascia over muscle bellies. Muscle spindles lie within the endomysium and perimysium, encased in a connective tissue capsule in parallel with a group of muscle fascicles, whereas at the muscle-tendon junction we can find more Golgi tendon organs.
Therefore, because these mechanoreceptors are embedded within fascia, any impediment to gliding between endofascial fibres and interfascial planes could cause anomalous tension and subsequent altered proprioceptive afferents. This could trigger faulty movement patterns at joints. Furthermore, over a certain threshold, all receptors can potentially become algoceptors (i.e., pain receptors), with consequent propagation of nociceptive signals.
In the absence of normal physiological elasticity, receptors embedded within the fascia may also be in an active state even at rest. Any further stretching, even that produced by normal muscular contraction, could cause excessive stimulation with consequent propagation of nociceptive afferents.
MTC: Should fascia be given serious consideration when treating repetitive strain injuries (RSIs) and why?
JD: If we consider that muscles and fascia are functionally inseparable then it follows that fascia should play an important role in these dysfunctions. Interestingly, not all people exposed to the same continuous stress develop RSI injuries. This implicates that a tensional malfunctioning, either in the same region or in adjacent regions, is a probable component in RSI syndromes. Fascia is a malleable tissue composed of collagen fibre bundles and elastic fibres. Overuse or repetitive strain causes repeated inflammation, resulting in changes in stiffness with disorientation of the collagen fibre bundles. Manual therapy can potentially restore elasticity/malleability to this tissue and re-establish correct tensional interplay between muscles and their fascia. In RSI injuries, it is often important to look beyond the local area of strain, questioning our clients carefully about past injuries in order to identify areas that may have never resolved completely in terms of fascial gliding.
MTC: We (clinicians) can see and feel changes in our client’s body in response to treatment, but what is actually happening beneath our hands? What is fascia’s response to manual manipulation – what can our hands influence?
JD: This is a big question that requires further studies. The perception of altered segmental tissue texture and its modification during therapy is a daily experience for most manual therapists.
Fascia demonstrates viscoelasticity, a material property whereby the deformation (strain) that results from a load (stress) will vary with changes in the rate and amount of loading. Loads within the elastic limits of the tissue will deform it but then it gradually returns to its original resting length after the load is removed. It is likely that a modified viscoelasticity of the extracellular matrix with subsequent misalignment of the endofascial collagen fibres will affect the fascia’s capacity to elongate and to adapt to stretch from muscle fibres.
By applying localized friction in an area of palpable rigidity, therapists create local heat, and this may increase certain chemical reactions within tissues such as reduced secretion of inflammatory cytokines. The redistribution of water from the tissue to the anatomical spaces surrounding the tissue also appears to be involved. This change in viscosity seems to involve an increase in the production of hyaluronic acid, one of the components of the matrix that has interesting intrinsic anti-inflammatory capacities. Improved drainage of inflammatory mediators and metabolic wastes probably contribute to the changes we feel under our hands by reducing chemical irritation of the various receptors in the tissue.
Hopefully, we will gain a lot more information about this subject at the next Fascia Research Congress!
Cathy Ryan has maintained a diverse, treatment-oriented massage therapy practice, and an extensive postgraduate training roster, since 1990. She is a long-standing member of the OMTA and has served as a subject matter expert, examiner and examiner trainer at the CMTO’s provincial licensing examinations. Ryan is the managing and commissioning editor for TouchU.ca, which provides education for touch professionals, students and the public. She is available to teach workshops and can be reached at: cryanrmt@gmail.com or
www.touchu.ca.
Print this page